-
PDF
- Split View
-
Views
-
Cite
Cite
Robert Sheldon, Sarah Rose, Stuart Connolly, Debbie Ritchie, Mary-Lou Koshman, Michael Frenneaux, for the Syncope Symptom Study Investigators, Diagnostic criteria for vasovagal syncope based on a quantitative history, European Heart Journal, Volume 27, Issue 3, February 2006, Pages 344–350, https://doi.org/10.1093/eurheartj/ehi584
Close - Share Icon Share
Abstract
Aims Our goal was to develop historical criteria for the diagnosis of vasovagal syncope.
Methods and results We administered a 118-item historical questionnaire to 418 patients with syncope and no apparent structural heart disease. The prevalence of each item was compared between patients with positive tilt tests and those with syncope of other, known causes. The contributions of symptoms to diagnoses were estimated with logistic regression, point scores were developed, and the scores were tested using receiver operator characteristic analysis. The accuracy of the decision rule was assessed with bootstrapping. Data sets were complete for all subjects. The causes of syncope were known in 323 patients and included tilt-positive vasovagal syncope (235 patients) and other diagnoses such as complete heart block and supraventricular tachycardias (88 patients). The point score correctly classified 90% of patients, diagnosing vasovagal syncope with 89% sensitivity and 91% specificity. The decision rule suggested that 68% of an additional 95 patients with syncope of unknown cause and a negative tilt test have vasovagal syncope.
Conclusion A simple point score of historical features distinguishes vasovagal syncope from syncope of other causes with very high sensitivity and specificity.
See page 253 for the editorial comment on this article (doi:10.1093/eurheartj/ehi663)
Introduction
Vasovagal syncope is the most common cause of syncope and can be troublesome to diagnose. As with other causes of total loss of consciousness, patients have no recollection of their unconsciousness, and the reliability of the diagnosis of the first loss of consciousness is quite low1. Many causes of syncope, although uncommon, have a treatable cause and/or an eventual poor outcome, while vasovagal syncope is not associated with excess mortality. The concern about identifying treatable arrhythmic and other causes, and for some causes, an eventual poor outcome2 coupled with the diagnostic uncertainty based upon the history has led to aggressive investigations of patients with syncope. Frequently, these are expensive,3,4 invasive, and all too commonly inaccurate or inefficient.5–8 Although the cause of syncope is eventually discovered in most patients who are referred to specialists, there is a need for a simple diagnostic tool for other settings. These might include primary care offices and emergency wards, and in epidemiologic, therapeutic, and health services studies. In these contexts, the current diagnostic tool, tilt testing, may not be feasible.
We aimed to develop simple diagnostic criteria for distinguishing vasovagal syncope from other causes of syncope in patients with structurally normal hearts, on the basis of a careful history targeted at specific features. We began with patients having positive tilt tests, as is the current conventional practice. We prospectively administered a structured questionnaire to syncope patients with a positive tilt test and quantitatively compared the responses with those of patients with syncope due to other known causes.9 From this, we developed a diagnostic point score to discriminate vasovagal syncope from syncope with other known causes.
Methods
Syncope symptom study
The University of Calgary Conjoint Medical Ethics Review Committee and similar committees in all participating centres approved this study. Patients were enrolled in Calgary, Canada; Hamilton, Canada; and Cardiff, United Kingdom.
Inclusion criteria
Consenting patients were eligible if they had had one or more loss of consciousness. They were recruited from sequentially identified patients in university and private practice cardiology clinics, pacemaker clinics, arrhythmia and syncope clinics, and hospital cardiology wards. They were included in the Syncope Symptom Study if they had a diagnosis established according to preset criteria (discussed subsequently), if there was no reasonable diagnostic confusion, or if reasonable investigations failed to elicit a diagnosis. That is, they were included if the diagnosis was known, or unknown despite reasonable attempts to elucidate one.
Exclusion criteria
Patients were excluded if they refused consent, were incapable of completing the questionnaire, or had more than one plausible cause of one syncopal spell. Patients with a history of known or suspected cardiomyopathy, or prior myocardial infarction, had the cardiac diagnosis confirmed by echocardiography, gated angiography, or cardiac catheterization, and were then excluded. The purpose of the larger study, the Syncope Symptom Study, was to develop historical diagnostic criteria for several classes of loss of consciousness.9 There were 671 subjects, of whom 102 had epileptic seizures and 151 had syncope in the setting of structural heart disease. The remaining 418 patients with syncope in the apparent absence of structural heart disease are the subjects of this report.
Gold standard diagnostic criteria
Patients had vasovagal syncope if they had a positive tilt test performed according to one of several currently acceptable methods.10–14 We chose not to specify that a particular tilt test protocol be used. This might have increased the internal validity of the study, but because each protocol has its own specificity and positive yield, we left the particular protocol up to the participating centre to increase external validity. It was deemed positive if it induced clinically reminiscent pre-syncope or syncope, and hypotension, bradycardia, or both. The specific degree of hypotension and bradycardia were pre-specified and depended on the protocol. These and other gold standard diagnostic criteria are listed in Table 1. All patients without an otherwise proven cause of syncope had an ECG and a tilt table test. Patients ≥60 years old usually underwent ambulatory electrocardiography.
Syncope symptom questionnaire
All patients completed a structured questionnaire9 with 118 items developed from that of Calkins et al.17 It assessed symptom burden, provocative situations, peri-syncopal symptoms, symptoms thought to be diagnostic of seizures, signs observed by bystanders, and relevant medical history. Completed questionnaires were checked for completion by study co-ordinators, and incomplete questionnaires were returned for revision. We cross-checked for incompatible entries to assess the accuracy of questionnaire completion.
Study definitions
In this article, we use working definitions, rather than pre-emptorily linking tilt test results to the term vasovagal syncope. Primary syncope denotes syncope of no apparent other cause in patients with either a positive tilt test (tilt-positive primary syncope) or a negative tilt test (tilt-negative primary syncope). Secondary syncope denotes syncope due to a known cause other than vasovagal syncope. We developed a point score that discriminated patients with primary tilt-positive syncope from patients with secondary syncope.
Statistical analysis9
First, we compared the prevalence of each variable in the tilt-positive primary syncope and secondary syncope groups using a Fisher's exact test and calculated the likelihood ratio for predicting the diagnosis of tilt-positive primary syncope. The likelihood ratio of each variable is its prevalence in the tilt-positive primary syncope group divided by its prevalence in the secondary syncope group. A variable with a likelihood ratio >1 is predictive of tilt-positive primary syncope and a variable with a ratio <1 is predictive of secondary syncope. Binary variables were created from continuous variables using a cut-point, which was the mean of the entire sample for symmetrically distributed variables and the median for variable that were very skewed. Variables with a very low prevalence were combined into a composite variable provided that both the magnitude and significance of the likelihood ratio were about the same and that the combination made clinical sense. Variables with similar meanings and similar descriptive statistics were also combined in order to reduce the number of variables eligible for inclusion in the following logistic regression analysis.
We then developed a manual stepwise logistic regression model that predicted tilt-positive primary syncope. Variables were eligible for inclusion in the logistic regression model if they were significant predictors (P<0.01) in the univariate analysis and were retained in the multivariable model if P<0.05 for the Wald statistic. No interactions between the variables were assessed.
To derive a practical diagnostic decision rule, a point score was developed by assigning ±1, ±2, ±3 (and so on) points to each of the factors based on the relative magnitude of the estimated regression coefficient. Each coefficient was divided by the smallest absolute value of the coefficient retained in the model, then rounded to the nearest integer. The points were summed and a diagnostic threshold chosen using receiver operating characteristic analysis.18 Using the diagnostic threshold, the apparent sensitivity, specificity, and overall accuracy in this test sample were estimated.
When the predictive accuracy of a diagnostic decision rule is assessed using the same patients from whom it was developed, an unduly optimistic classification rate might occur.19 This is referred to as the apparent accuracy. Ideally, the true accuracy should be evaluated using a split sample,9 but in this case, our sample size for the secondary syncope group was not large enough. Accordingly, we used a bootstrap analysis to estimate the excess error that would be detected if an independent sample was used to evaluate the diagnostic accuracy.19 Five thousand bootstrap samples were drawn from the original sample. For each bootstrap sample, the logistic regression model with the same variables as those in the adopted model was fitted to re-estimate the regression coefficients and the diagnostic decision rule developed. The accuracy of the new decision rule from the bootstrap sample was then assessed in the original sample. The expected excess error rate was calculated from the 5000 bootstrap samples, then subtracted from the apparent accuracy to obtain estimates of the true sensitivity, specificity, and overall accuracy of the diagnostic decision rule.
We derived classification rules both with and without the variables of symptom burden and durations. Finally, we compared the symptoms of patients with gold standard diagnoses with those with no identifiable cause of syncope by two methods. First, we determined the diagnostic performance of the point score for tilt-positive primary syncope in patients with tilt-negative primary syncope. Secondly, we compared the tilt-positive primary syncope patients with tilt-negative primary syncope patients, both of whom fit the derived diagnostic criteria for tilt-positive primary syncope.
Results
Patient population (Table 2)
Patient enrolment occurred between January 1995 and July 2001. All patients who were approached consented, and only two were disqualified, because they had more than one plausible cause of syncope. There were 235 patients with syncope and positive tilt tests (tilt-positive primary syncope), 95 patients with no apparent cause of syncope and negative tilt tests (tilt-negative primary syncope), and 88 patients with other identified causes of syncope (secondary syncope). Of the latter, 42 had complete heart block, 21 had a supraventricular tachycardia, six had idiopathic ventricular tachycardia, five had aortic stenosis, three had Torsades de Pointe ventricular tachycardia, cough syncope, or hypersensitive carotid sinus syncope, two had pulmonary emboli, and one had ischaemic ventricular tachycardia, hyperventilation syncope, or autonomic neuropathy. The tilt-positive primary syncope patients were younger than the secondary syncope patients, and more were women. The tilt-positive primary syncope patients had had more syncopal spells than the secondary syncope patients (P<0.001). Symptoms were present in the tilt-positive primary syncope patients over a longer duration of time (P<0.001) compared with the secondary syncope patients. The mean age for the tilt-negative primary syncope patients was 49±21 years, and 54% were women. They had a median five syncope spells (IQR 3–12) over a median 29 months (IQR 3–132).
Classification score
The most important univariate features that distinguish between patients with tilt-positive primary syncope and with secondary syncope are presented in Table 3. Of the original 118 items, 71 were significantly predictors of primary vs. secondary syncope at P<0.05. These 71 variables were reduced to 34 variables by appropriate combination as described earlier, and descriptive information is presented in Table 3. These 34 variables were eligible for inclusion in the logistic regression model, seven of which were included in the final model. After including these seven variables in the multivariable logistic regression model, none of the remaining variables were significant at P<0.05.
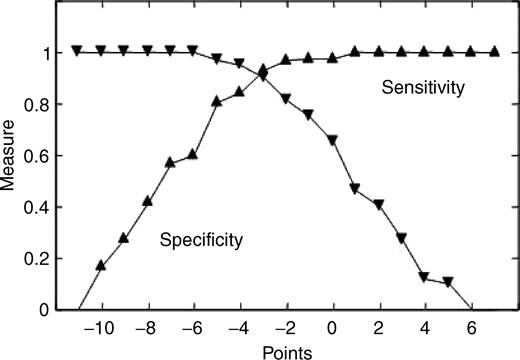
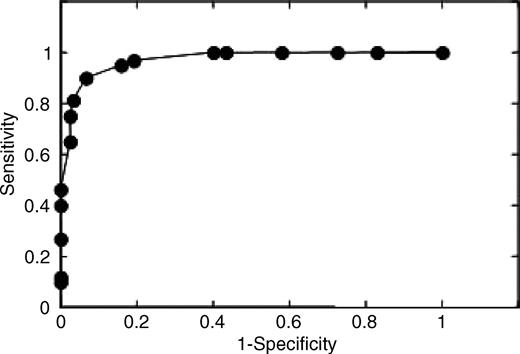
Features were included in the table if the likelihood ratio (see Methods) was >1.0 (predictive of tilt-positive primary syncope) or <1.0 (predictive of secondary syncope) with P≤0.05. A diagnostic point score was derived from the relative weighting of the regression coefficients without inclusion of estimates of symptom burden (Table 4). The diagnostic behaviour of this point score is illustrated in Figure 1. Patients were classified as having tilt-positive primary syncope if the point score was ≥−2. This resulted in an apparent overall accuracy of 91%, apparent sensitivity of 90%, and apparent specificity of 93% (Figure 2). When the bootstrap estimates of excess error were included, the true overall accuracy was 89.7%, with a true sensitivity of 89.3% and a true specificity of 90.8%.
Features of the history that contributed to the diagnosis of tilt-positive primary syncope included pre-syncope or syncope with exposure to pain or a medical procedure, diaphoresis or perceived warmth before a spell, and pre-syncope or syncope with prolonged sitting or standing. Factors that were strongly predictive of syncope secondary to other causes included known bifascicular block, asystole, supraventricular tachycardia, or diabetes; observed cyanosis; a memory of the spell; and older age at onset of syncope. The measures of symptom burden were non-significant after including the aforementioned variables in the model and did not improve the diagnostic ability of the model.
Syncope of unknown cause
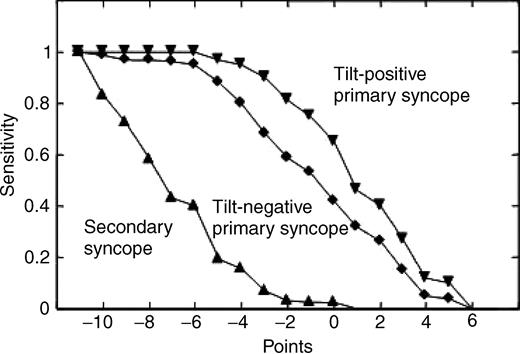
The diagnostic scheme classified 68% of patients with tilt-negative primary syncope as though they had tilt-positive primary syncope. The similar distributions of the point scores in the tilt-negative and tilt-positive primary syncope patients when compared with the patients with secondary syncope are shown in Figure 3. Finally, we assessed whether any of the 71 original significant predictors discriminated between patients whose point scores were ≥−2, and who had either positive or negative tilt tests. Only four out of 71 variables were statistically significant, with P=0.014–0.049. When 71 independent tests are performed, the probability of four or more being significant due to chance alone at the 5% level of significance is 0.48, indicating that there is little evidence of any significant difference between these two groups. Similarly, only two of the 34 variables presented in Table 3 were significant at P<0.05.
Discussion
Clinical implications
In patients with a transient loss of consciousness, there is substantial diagnostic disagreement among physicians, and written diagnostic criteria improve inter-rater agreement.1,20 Although tilt table testing has provided important diagnostic and physiologic insights, it is not readily available in emergency wards and family physicians' offices, and by codifying diagnosis, the score may streamline management. Similarly, tilt testing may not be feasible in larger community-based studies of people with syncope who are not patients. Varying the diagnostic cut-off level would allow investigators to vary the sensitivity, specificity, and predictive values of the score depending on the need of the study.
The point score was developed from structured questionnaires prospectively administered to patients with apparently structurally normal hearts, and not from a post hoc chart review. Tilt tests were selected as the entry point for patients with presumed vasovagal syncope, because the tilt table test was developed to mimic some of the physiology of vasovagal syncope; they provoke symptoms reminiscent of the patients' syncopal spells; and because positive tilt tests are accompanied by hypotension and bradycardia, as is vasovagal syncope.
Features of questionnaire
The classification scheme is simple, and to some extent confirms previous empiric diagnostic criteria. We present derived diagnostic questions and their points in Table 5. The patient has vasovagal syncope if the point score is ≥−2 and syncope due to other causes if the point score is <−2. Some of the diagnostic factors in favour of vasovagal syncope in the model reflect the situations in which vasovagal syncope occurs. These include prolonged sitting or standing and exposure to medical situations. The age criterion reflects the young age at which vasovagal syncope usually first occurs.
However, these used alone were not necessarily sufficient. Four risk factors for other causes of syncope, asystole or bifascicular block on an ECG, supraventricular tachycardia, and diabetes, usually need to be absent to establish a diagnosis of vasovagal syncope. The classification scheme was not improved with the addition of the criteria for the duration of the history or number of syncopal spells. This suggests that patients can be accurately diagnosed at first presentation and that health care wait lists do not confound the diagnosis.
Other studies
Calkins et al.17 reported a prospective, evidence-based study of the symptoms of patients with ventricular tachycardia, complete heart block, or tilt test-positive vasovagal syncope. Most patients had structural heart disease. Alboni et al.21 reported symptoms in 341 unselected syncope patients, many of whom had structural heart disease. The study was aimed at diagnosing cardiac causes of syncope, and a history of heart disease was the most important factor. Although there were highly significant differences in symptom distribution among the diagnostic groups in the preceding two reports, the results did not culminate in diagnostic point scores.
Negative and positive tilts
The close symptomatic similarity between most patients with negative and positive tilt tests is consistent with the idea that most patients with negative tilt tests have falsely negative tests. Given that the score is 90% sensitive for tilt-positive primary syncope, and that 68% of tilt-negative primary syncope patients fall in the same diagnostic category, it may be that up to 76% of tilt-negative primary syncope patients truly have vasovagal syncope. Patients with negative and positive tests have similar symptom burdens, similar clinical outcomes in the 3 years following the tilt test, and behave similarly in a multivariable predictive model of pre-test variables for post-test outcome.22–24
Limitations
Patients were accrued from tertiary care clinics and acute care facilities, and these findings need to be tested in a broadly based population. There may be some patients with rare presentations of common disorders who went undiagnosed. We did not specify a particular tilt test protocol to be used. Although this might have increased the internal validity of the study, we recognized that each protocol has its own specificity and positive yield, and therefore, left the particular protocol up to the participating centre to increase external validity. Similarly, we did not specify the investigations necessary to diagnose the absence of structural heart disease. By leaving this to individual centres, we hoped to derive diagnostic criteria driven by and relevant to conventional clinical practice. We assessed the optimism error of the diagnostic schemes with bootstrapping, and independent confirmation is desirable. These criteria should be tested in relatively uncommon syndromes such as long QT syndrome and Brugada syndrome. Another strategy to the development of a diagnostic point score would have been to develop it using subjects with what are assumed to be classic histories of vasovagal syncope, but these criteria are not evidence-based and might be self-fulfilling. Accordingly, we started with tilt test criteria and worked independently towards a historical definition. We hoped this would avoid excessive bias. The point score may reflect regional and referral idiosyncrasies of the study population tested, as well as the particular tilt tests used. The limitations of tilt tests as diagnostic tools were reviewed recently.8 The questionnaire was administered to some patients after their relevant diagnostic studies, and this might have reinforced recollection of symptoms specific to the test outcomes. The effect of age on recollection of symptoms is unknown, as is the use of the point score in elderly patients. We do emphasize that the point score is applicable only to patients without structural heart disease. These concerns underlie the importance of assessing the accuracy and utility of the point score in other populations and settings. Indeed, it has been used in a population-based survey of syncope, is an inclusion measure in an ongoing multinational randomized clinical trial, and will be used in upcoming epidemiological studies in community and acute care sectors. Clinicians should use these criteria only as a guide to diagnosis.
Acknowledgement
This study was funded by Medtronic, Toronto, Ontario, Canada; the Calgary General Hospital Volunteers Foundation; and the Canadian Institutes for Health Research, Ottawa, Ontario, Canada.
Conflict of interest: none declared.
Appendix
The following investigators participated: University of Calgary, Calgary, Alberta: R. Sheldon, D. Ritchie, M. Koshman, B. Mitchell, D. Wyse, H.J. Duff, A. Gillis, M.A. Lee, W.F. Murphy; Hamilton Health Sciences Corporation, Hamilton, Ontario: S. Connolly; Wales Heart Institute, Cardiff, Wales: M. Frenneaux, J. Pascual. St Michael's Hospital, Toronto, Ontario: D. Newman. The steering committee consisted of Dr Sheldon, Dr S Rose, and Ms Ritchie.
The Syncope Symptom Study Investigators are listed in the Appendix.
Figure 1 Sensitivity and specificity for the diagnosis of tilt-positive primary syncope compared with secondary syncope using the point scores reported in Table 2.
Figure 2 Receiver operator characteristic analysis of the diagnostic score developed in Table 2. The populations are those of patients with primary tilt-positive syncope and patients with secondary syncope.
Figure 3 A comparison of point score distributions for populations of tilt-positive and tilt-negative primary syncope patients.
Gold standard diagnostic criteria for patient inclusion and working diagnostic definitions used in this study during analysis
| Diagnosis . | Definition . |
|---|---|
| Gold standard diagnoses | |
| Vasovagal syncope | Positive tilt test using a currently acceptable method10–14 |
| Ventricular tachycardia | Sustained VT documented during syncope, or ≤48 h of admission for syncope, or if haemodynamically unstable, sustained monomorphic VT was induced during an electrophysiologic study15 |
| Torsade de Pointes | Documented at the time of syncope or shortly afterwards with classic clinical features |
| Supraventricular tachycardia | Established diagnosis of arrhythmia, and typical palpitations immediately preceding a syncopal spell, or awoke from syncope with those symptoms |
| Complete heart block | Complete heart block with a wide QRS escape rhythm documented during syncope or shortly afterwards |
| Orthostatic hypotension | Documented autonomic neuropathy with significant orthostatic hypotension and presyncope or syncope during tilt table testing16 |
| Working diagnostic definitions during analysis | |
| Primary syncope | Syncope of no apparent other cause with either a positive tilt test (tilt-positive primary syncope) or negative tilt test (tilt-negative primary syncope) |
| Secondary syncope | Syncope due to a known cause other than vasovagal syncope |
| Diagnosis . | Definition . |
|---|---|
| Gold standard diagnoses | |
| Vasovagal syncope | Positive tilt test using a currently acceptable method10–14 |
| Ventricular tachycardia | Sustained VT documented during syncope, or ≤48 h of admission for syncope, or if haemodynamically unstable, sustained monomorphic VT was induced during an electrophysiologic study15 |
| Torsade de Pointes | Documented at the time of syncope or shortly afterwards with classic clinical features |
| Supraventricular tachycardia | Established diagnosis of arrhythmia, and typical palpitations immediately preceding a syncopal spell, or awoke from syncope with those symptoms |
| Complete heart block | Complete heart block with a wide QRS escape rhythm documented during syncope or shortly afterwards |
| Orthostatic hypotension | Documented autonomic neuropathy with significant orthostatic hypotension and presyncope or syncope during tilt table testing16 |
| Working diagnostic definitions during analysis | |
| Primary syncope | Syncope of no apparent other cause with either a positive tilt test (tilt-positive primary syncope) or negative tilt test (tilt-negative primary syncope) |
| Secondary syncope | Syncope due to a known cause other than vasovagal syncope |
Gold standard diagnostic criteria for patient inclusion and working diagnostic definitions used in this study during analysis
| Diagnosis . | Definition . |
|---|---|
| Gold standard diagnoses | |
| Vasovagal syncope | Positive tilt test using a currently acceptable method10–14 |
| Ventricular tachycardia | Sustained VT documented during syncope, or ≤48 h of admission for syncope, or if haemodynamically unstable, sustained monomorphic VT was induced during an electrophysiologic study15 |
| Torsade de Pointes | Documented at the time of syncope or shortly afterwards with classic clinical features |
| Supraventricular tachycardia | Established diagnosis of arrhythmia, and typical palpitations immediately preceding a syncopal spell, or awoke from syncope with those symptoms |
| Complete heart block | Complete heart block with a wide QRS escape rhythm documented during syncope or shortly afterwards |
| Orthostatic hypotension | Documented autonomic neuropathy with significant orthostatic hypotension and presyncope or syncope during tilt table testing16 |
| Working diagnostic definitions during analysis | |
| Primary syncope | Syncope of no apparent other cause with either a positive tilt test (tilt-positive primary syncope) or negative tilt test (tilt-negative primary syncope) |
| Secondary syncope | Syncope due to a known cause other than vasovagal syncope |
| Diagnosis . | Definition . |
|---|---|
| Gold standard diagnoses | |
| Vasovagal syncope | Positive tilt test using a currently acceptable method10–14 |
| Ventricular tachycardia | Sustained VT documented during syncope, or ≤48 h of admission for syncope, or if haemodynamically unstable, sustained monomorphic VT was induced during an electrophysiologic study15 |
| Torsade de Pointes | Documented at the time of syncope or shortly afterwards with classic clinical features |
| Supraventricular tachycardia | Established diagnosis of arrhythmia, and typical palpitations immediately preceding a syncopal spell, or awoke from syncope with those symptoms |
| Complete heart block | Complete heart block with a wide QRS escape rhythm documented during syncope or shortly afterwards |
| Orthostatic hypotension | Documented autonomic neuropathy with significant orthostatic hypotension and presyncope or syncope during tilt table testing16 |
| Working diagnostic definitions during analysis | |
| Primary syncope | Syncope of no apparent other cause with either a positive tilt test (tilt-positive primary syncope) or negative tilt test (tilt-negative primary syncope) |
| Secondary syncope | Syncope due to a known cause other than vasovagal syncope |
Clinical and demographic characteristics of three patient groups
| Characteristic . | Tilt-positive primary syncope . | Secondary syncope . | P-value, tilt-positive primary vs. secondary . | Tilt-negative primary syncope . |
|---|---|---|---|---|
| Number | 235 | 88 | 95 | |
| Age, years (mean, SD) | 42±18 | 63±16 | <0.001 | 49±21 |
| Females | 61% | 45% | 0.011 | 54% |
| Syncopal spells, n (Median, IQR) | 6 (3–20) | 2 (1–5) | <0.001 | 5 (3–12) |
| Symptom duration, months (Median, IQR) | 100 (13–268) | 1 (0–16) | <0.001 | 29 (3–132) |
| Characteristic . | Tilt-positive primary syncope . | Secondary syncope . | P-value, tilt-positive primary vs. secondary . | Tilt-negative primary syncope . |
|---|---|---|---|---|
| Number | 235 | 88 | 95 | |
| Age, years (mean, SD) | 42±18 | 63±16 | <0.001 | 49±21 |
| Females | 61% | 45% | 0.011 | 54% |
| Syncopal spells, n (Median, IQR) | 6 (3–20) | 2 (1–5) | <0.001 | 5 (3–12) |
| Symptom duration, months (Median, IQR) | 100 (13–268) | 1 (0–16) | <0.001 | 29 (3–132) |
Clinical and demographic characteristics of three patient groups
| Characteristic . | Tilt-positive primary syncope . | Secondary syncope . | P-value, tilt-positive primary vs. secondary . | Tilt-negative primary syncope . |
|---|---|---|---|---|
| Number | 235 | 88 | 95 | |
| Age, years (mean, SD) | 42±18 | 63±16 | <0.001 | 49±21 |
| Females | 61% | 45% | 0.011 | 54% |
| Syncopal spells, n (Median, IQR) | 6 (3–20) | 2 (1–5) | <0.001 | 5 (3–12) |
| Symptom duration, months (Median, IQR) | 100 (13–268) | 1 (0–16) | <0.001 | 29 (3–132) |
| Characteristic . | Tilt-positive primary syncope . | Secondary syncope . | P-value, tilt-positive primary vs. secondary . | Tilt-negative primary syncope . |
|---|---|---|---|---|
| Number | 235 | 88 | 95 | |
| Age, years (mean, SD) | 42±18 | 63±16 | <0.001 | 49±21 |
| Females | 61% | 45% | 0.011 | 54% |
| Syncopal spells, n (Median, IQR) | 6 (3–20) | 2 (1–5) | <0.001 | 5 (3–12) |
| Symptom duration, months (Median, IQR) | 100 (13–268) | 1 (0–16) | <0.001 | 29 (3–132) |
Comparison of the most significant historical features in patients with tilt-positive primary syncope compared with other known causes of syncope (secondary syncope)
| Variable . | Prevalence (%) . | Sensitivity (%) . | Specificity (%) . | LHR . | P-value . |
|---|---|---|---|---|---|
| Age at first syncopal spell ≤35 | 55.1 | 72.3 | 90.9 | 7.96 | <0.0001 |
| Less than 5 s warning | 46.1 | 38.7 | 34.1 | 0.59 | <0.0001 |
| Tired after syncopal spell | 80.8 | 87.2 | 36.4 | 1.37 | <0.0001 |
| Provocative situations | |||||
| Syncope/pre-syncope with pain or medical procedure | 36.5 | 48.1 | 94.3 | 8.46 | <0.0001 |
| Syncope/pre-syncope with hot or warm environments | 42.4 | 54.9 | 90.9 | 6.08 | <0.0001 |
| Syncope/pre-syncope with stress | 25.7 | 32.3 | 92.0 | 4.07 | <0.0001 |
| Syncope/pre-syncope with headaches | 23.2 | 30.2 | 95.5 | 6.65 | <0.0001 |
| Syncope/pre-syncope with prolonged sitting/standing | 60.7 | 69.4 | 62.5 | 1.85 | <0.0001 |
| Syncope/pre-syncope on the way to the toilet | 13.0 | 16.2 | 95.5 | 3.56 | 0.0099 |
| Syncope/pre-syncope after using the toilet | 7.7 | 10.6 | 100 | a | 0.0032 |
| Pre-syncope after exercise | 36.2 | 42.6 | 80.7 | 2.20 | 0.0002 |
| Behaviour during syncope | |||||
| Cannot remember behaviour during syncope | 14.2 | 17.9 | 95.5 | 3.93 | 0.0041 |
| Unresponsive during syncope | 31.6 | 39.6 | 89.8 | 3.87 | <0.0001 |
| No memory about syncope | 53.3 | 47.2 | 30.7 | 0.68 | 0.0006 |
| Confusion after a spell | 35.0 | 40.4 | 79.5 | 1.98 | 0.0013 |
| Cyanotic during syncope | 3.1 | 1.3 | 92.0 | 0.16 | 0.0064 |
| White or pale colour noted by bystander | 64.4 | 70.6 | 52.3 | 1.48 | 0.0002 |
| Medical history | |||||
| Valvular heart disease | 10.2 | 6.4 | 79.5 | 0.31 | 0.0004 |
| Atrial fibrillation or flutter | 4.6 | 1.7 | 87.5 | 0.14 | 0.0001 |
| Any one of bifascicular block, diabetes, supraventricular tachycardia, diabetes | 19.8 | 3.4 | 36.4 | 0.05 | <0.0001 |
| Hypertension | 18.0 | 11.1 | 63.3 | 0.30 | <0.001 |
| Perisyncopal symptoms | |||||
| Nausea or vomiting before a spell | 36.8 | 43.4 | 80.7 | 2.25 | 0.0001 |
| Sweating or warm feeling before a spell | 51.7 | 62.1 | 76.1 | 2.60 | <0.0001 |
| Headache before a spell | 15.2 | 19.6 | 96.6 | 5.74 | 0.0006 |
| Visual distortion before a spell | 47.4 | 53.6 | 69.3 | 1.75 | 0.0004 |
| Auditory distortion before a spell | 29.7 | 35.7 | 86.4 | 2.62 | 0.0002 |
| Heart racing before a spell | 39.6 | 45.5 | 76.1 | 1.91 | 0.0006 |
| Abdominal rising sensation | 12.7 | 16.2 | 96.6 | 4.74 | 0.0040 |
| Numbness or tingling before a spell | 22.6 | 27.7 | 90.9 | 3.04 | 0.0007 |
| Mood changes or pre-occupation before a spell | 18.3 | 24.3 | 97.7 | 10.67 | <0.0001 |
| Sweating or warm feeling after a spell | 33.4 | 40.0 | 84.1 | 2.51 | 0.0001 |
| Mood changes after a spell | 13.0 | 16.6 | 96.6 | 4.87 | 0.0032 |
| Numbness or tingling after a spell | 14.9 | 18.3 | 94.3 | 3.22 | 0.0078 |
| Nausea or vomiting after a spell | 28.5 | 35.3 | 89.8 | 3.45 | <0.0001 |
| Variable . | Prevalence (%) . | Sensitivity (%) . | Specificity (%) . | LHR . | P-value . |
|---|---|---|---|---|---|
| Age at first syncopal spell ≤35 | 55.1 | 72.3 | 90.9 | 7.96 | <0.0001 |
| Less than 5 s warning | 46.1 | 38.7 | 34.1 | 0.59 | <0.0001 |
| Tired after syncopal spell | 80.8 | 87.2 | 36.4 | 1.37 | <0.0001 |
| Provocative situations | |||||
| Syncope/pre-syncope with pain or medical procedure | 36.5 | 48.1 | 94.3 | 8.46 | <0.0001 |
| Syncope/pre-syncope with hot or warm environments | 42.4 | 54.9 | 90.9 | 6.08 | <0.0001 |
| Syncope/pre-syncope with stress | 25.7 | 32.3 | 92.0 | 4.07 | <0.0001 |
| Syncope/pre-syncope with headaches | 23.2 | 30.2 | 95.5 | 6.65 | <0.0001 |
| Syncope/pre-syncope with prolonged sitting/standing | 60.7 | 69.4 | 62.5 | 1.85 | <0.0001 |
| Syncope/pre-syncope on the way to the toilet | 13.0 | 16.2 | 95.5 | 3.56 | 0.0099 |
| Syncope/pre-syncope after using the toilet | 7.7 | 10.6 | 100 | a | 0.0032 |
| Pre-syncope after exercise | 36.2 | 42.6 | 80.7 | 2.20 | 0.0002 |
| Behaviour during syncope | |||||
| Cannot remember behaviour during syncope | 14.2 | 17.9 | 95.5 | 3.93 | 0.0041 |
| Unresponsive during syncope | 31.6 | 39.6 | 89.8 | 3.87 | <0.0001 |
| No memory about syncope | 53.3 | 47.2 | 30.7 | 0.68 | 0.0006 |
| Confusion after a spell | 35.0 | 40.4 | 79.5 | 1.98 | 0.0013 |
| Cyanotic during syncope | 3.1 | 1.3 | 92.0 | 0.16 | 0.0064 |
| White or pale colour noted by bystander | 64.4 | 70.6 | 52.3 | 1.48 | 0.0002 |
| Medical history | |||||
| Valvular heart disease | 10.2 | 6.4 | 79.5 | 0.31 | 0.0004 |
| Atrial fibrillation or flutter | 4.6 | 1.7 | 87.5 | 0.14 | 0.0001 |
| Any one of bifascicular block, diabetes, supraventricular tachycardia, diabetes | 19.8 | 3.4 | 36.4 | 0.05 | <0.0001 |
| Hypertension | 18.0 | 11.1 | 63.3 | 0.30 | <0.001 |
| Perisyncopal symptoms | |||||
| Nausea or vomiting before a spell | 36.8 | 43.4 | 80.7 | 2.25 | 0.0001 |
| Sweating or warm feeling before a spell | 51.7 | 62.1 | 76.1 | 2.60 | <0.0001 |
| Headache before a spell | 15.2 | 19.6 | 96.6 | 5.74 | 0.0006 |
| Visual distortion before a spell | 47.4 | 53.6 | 69.3 | 1.75 | 0.0004 |
| Auditory distortion before a spell | 29.7 | 35.7 | 86.4 | 2.62 | 0.0002 |
| Heart racing before a spell | 39.6 | 45.5 | 76.1 | 1.91 | 0.0006 |
| Abdominal rising sensation | 12.7 | 16.2 | 96.6 | 4.74 | 0.0040 |
| Numbness or tingling before a spell | 22.6 | 27.7 | 90.9 | 3.04 | 0.0007 |
| Mood changes or pre-occupation before a spell | 18.3 | 24.3 | 97.7 | 10.67 | <0.0001 |
| Sweating or warm feeling after a spell | 33.4 | 40.0 | 84.1 | 2.51 | 0.0001 |
| Mood changes after a spell | 13.0 | 16.6 | 96.6 | 4.87 | 0.0032 |
| Numbness or tingling after a spell | 14.9 | 18.3 | 94.3 | 3.22 | 0.0078 |
| Nausea or vomiting after a spell | 28.5 | 35.3 | 89.8 | 3.45 | <0.0001 |
The behaviour of each of the variables is expressed in terms of the prevalence in the sample, sensitivity, specificity, and likelihood ratio for tilt-positive primary syncope, as diagnosed by a positive tilt table test. LHR, likelihood ratio.
aThe likelihood ratio cannot be calculated because the specificity is equal to 100%.
Comparison of the most significant historical features in patients with tilt-positive primary syncope compared with other known causes of syncope (secondary syncope)
| Variable . | Prevalence (%) . | Sensitivity (%) . | Specificity (%) . | LHR . | P-value . |
|---|---|---|---|---|---|
| Age at first syncopal spell ≤35 | 55.1 | 72.3 | 90.9 | 7.96 | <0.0001 |
| Less than 5 s warning | 46.1 | 38.7 | 34.1 | 0.59 | <0.0001 |
| Tired after syncopal spell | 80.8 | 87.2 | 36.4 | 1.37 | <0.0001 |
| Provocative situations | |||||
| Syncope/pre-syncope with pain or medical procedure | 36.5 | 48.1 | 94.3 | 8.46 | <0.0001 |
| Syncope/pre-syncope with hot or warm environments | 42.4 | 54.9 | 90.9 | 6.08 | <0.0001 |
| Syncope/pre-syncope with stress | 25.7 | 32.3 | 92.0 | 4.07 | <0.0001 |
| Syncope/pre-syncope with headaches | 23.2 | 30.2 | 95.5 | 6.65 | <0.0001 |
| Syncope/pre-syncope with prolonged sitting/standing | 60.7 | 69.4 | 62.5 | 1.85 | <0.0001 |
| Syncope/pre-syncope on the way to the toilet | 13.0 | 16.2 | 95.5 | 3.56 | 0.0099 |
| Syncope/pre-syncope after using the toilet | 7.7 | 10.6 | 100 | a | 0.0032 |
| Pre-syncope after exercise | 36.2 | 42.6 | 80.7 | 2.20 | 0.0002 |
| Behaviour during syncope | |||||
| Cannot remember behaviour during syncope | 14.2 | 17.9 | 95.5 | 3.93 | 0.0041 |
| Unresponsive during syncope | 31.6 | 39.6 | 89.8 | 3.87 | <0.0001 |
| No memory about syncope | 53.3 | 47.2 | 30.7 | 0.68 | 0.0006 |
| Confusion after a spell | 35.0 | 40.4 | 79.5 | 1.98 | 0.0013 |
| Cyanotic during syncope | 3.1 | 1.3 | 92.0 | 0.16 | 0.0064 |
| White or pale colour noted by bystander | 64.4 | 70.6 | 52.3 | 1.48 | 0.0002 |
| Medical history | |||||
| Valvular heart disease | 10.2 | 6.4 | 79.5 | 0.31 | 0.0004 |
| Atrial fibrillation or flutter | 4.6 | 1.7 | 87.5 | 0.14 | 0.0001 |
| Any one of bifascicular block, diabetes, supraventricular tachycardia, diabetes | 19.8 | 3.4 | 36.4 | 0.05 | <0.0001 |
| Hypertension | 18.0 | 11.1 | 63.3 | 0.30 | <0.001 |
| Perisyncopal symptoms | |||||
| Nausea or vomiting before a spell | 36.8 | 43.4 | 80.7 | 2.25 | 0.0001 |
| Sweating or warm feeling before a spell | 51.7 | 62.1 | 76.1 | 2.60 | <0.0001 |
| Headache before a spell | 15.2 | 19.6 | 96.6 | 5.74 | 0.0006 |
| Visual distortion before a spell | 47.4 | 53.6 | 69.3 | 1.75 | 0.0004 |
| Auditory distortion before a spell | 29.7 | 35.7 | 86.4 | 2.62 | 0.0002 |
| Heart racing before a spell | 39.6 | 45.5 | 76.1 | 1.91 | 0.0006 |
| Abdominal rising sensation | 12.7 | 16.2 | 96.6 | 4.74 | 0.0040 |
| Numbness or tingling before a spell | 22.6 | 27.7 | 90.9 | 3.04 | 0.0007 |
| Mood changes or pre-occupation before a spell | 18.3 | 24.3 | 97.7 | 10.67 | <0.0001 |
| Sweating or warm feeling after a spell | 33.4 | 40.0 | 84.1 | 2.51 | 0.0001 |
| Mood changes after a spell | 13.0 | 16.6 | 96.6 | 4.87 | 0.0032 |
| Numbness or tingling after a spell | 14.9 | 18.3 | 94.3 | 3.22 | 0.0078 |
| Nausea or vomiting after a spell | 28.5 | 35.3 | 89.8 | 3.45 | <0.0001 |
| Variable . | Prevalence (%) . | Sensitivity (%) . | Specificity (%) . | LHR . | P-value . |
|---|---|---|---|---|---|
| Age at first syncopal spell ≤35 | 55.1 | 72.3 | 90.9 | 7.96 | <0.0001 |
| Less than 5 s warning | 46.1 | 38.7 | 34.1 | 0.59 | <0.0001 |
| Tired after syncopal spell | 80.8 | 87.2 | 36.4 | 1.37 | <0.0001 |
| Provocative situations | |||||
| Syncope/pre-syncope with pain or medical procedure | 36.5 | 48.1 | 94.3 | 8.46 | <0.0001 |
| Syncope/pre-syncope with hot or warm environments | 42.4 | 54.9 | 90.9 | 6.08 | <0.0001 |
| Syncope/pre-syncope with stress | 25.7 | 32.3 | 92.0 | 4.07 | <0.0001 |
| Syncope/pre-syncope with headaches | 23.2 | 30.2 | 95.5 | 6.65 | <0.0001 |
| Syncope/pre-syncope with prolonged sitting/standing | 60.7 | 69.4 | 62.5 | 1.85 | <0.0001 |
| Syncope/pre-syncope on the way to the toilet | 13.0 | 16.2 | 95.5 | 3.56 | 0.0099 |
| Syncope/pre-syncope after using the toilet | 7.7 | 10.6 | 100 | a | 0.0032 |
| Pre-syncope after exercise | 36.2 | 42.6 | 80.7 | 2.20 | 0.0002 |
| Behaviour during syncope | |||||
| Cannot remember behaviour during syncope | 14.2 | 17.9 | 95.5 | 3.93 | 0.0041 |
| Unresponsive during syncope | 31.6 | 39.6 | 89.8 | 3.87 | <0.0001 |
| No memory about syncope | 53.3 | 47.2 | 30.7 | 0.68 | 0.0006 |
| Confusion after a spell | 35.0 | 40.4 | 79.5 | 1.98 | 0.0013 |
| Cyanotic during syncope | 3.1 | 1.3 | 92.0 | 0.16 | 0.0064 |
| White or pale colour noted by bystander | 64.4 | 70.6 | 52.3 | 1.48 | 0.0002 |
| Medical history | |||||
| Valvular heart disease | 10.2 | 6.4 | 79.5 | 0.31 | 0.0004 |
| Atrial fibrillation or flutter | 4.6 | 1.7 | 87.5 | 0.14 | 0.0001 |
| Any one of bifascicular block, diabetes, supraventricular tachycardia, diabetes | 19.8 | 3.4 | 36.4 | 0.05 | <0.0001 |
| Hypertension | 18.0 | 11.1 | 63.3 | 0.30 | <0.001 |
| Perisyncopal symptoms | |||||
| Nausea or vomiting before a spell | 36.8 | 43.4 | 80.7 | 2.25 | 0.0001 |
| Sweating or warm feeling before a spell | 51.7 | 62.1 | 76.1 | 2.60 | <0.0001 |
| Headache before a spell | 15.2 | 19.6 | 96.6 | 5.74 | 0.0006 |
| Visual distortion before a spell | 47.4 | 53.6 | 69.3 | 1.75 | 0.0004 |
| Auditory distortion before a spell | 29.7 | 35.7 | 86.4 | 2.62 | 0.0002 |
| Heart racing before a spell | 39.6 | 45.5 | 76.1 | 1.91 | 0.0006 |
| Abdominal rising sensation | 12.7 | 16.2 | 96.6 | 4.74 | 0.0040 |
| Numbness or tingling before a spell | 22.6 | 27.7 | 90.9 | 3.04 | 0.0007 |
| Mood changes or pre-occupation before a spell | 18.3 | 24.3 | 97.7 | 10.67 | <0.0001 |
| Sweating or warm feeling after a spell | 33.4 | 40.0 | 84.1 | 2.51 | 0.0001 |
| Mood changes after a spell | 13.0 | 16.6 | 96.6 | 4.87 | 0.0032 |
| Numbness or tingling after a spell | 14.9 | 18.3 | 94.3 | 3.22 | 0.0078 |
| Nausea or vomiting after a spell | 28.5 | 35.3 | 89.8 | 3.45 | <0.0001 |
The behaviour of each of the variables is expressed in terms of the prevalence in the sample, sensitivity, specificity, and likelihood ratio for tilt-positive primary syncope, as diagnosed by a positive tilt table test. LHR, likelihood ratio.
aThe likelihood ratio cannot be calculated because the specificity is equal to 100%.
Point scores for the diagnosis of tilt-positive primary syncope, in the absence of knowledge of the numbers and historical duration of syncope and pre-syncope
| . | Regression coefficient (SE) . | P-value . | Points . |
|---|---|---|---|
| Any one of bifascicular block, asystole, supraventricular tachycardia, diabetes | −4.93 (0.76) | <0.001 | −5 |
| Blue colour noted by bystander | −4.19 (1.26) | <0.001 | −4 |
| Age at first syncope ≥35 years | −2.61 (0.63) | <0.001 | −3 |
| Remembers something about the spell | −1.80 (0.53) | <0.001 | −2 |
| Pre-syncope or syncope with prolonged sitting or standing | 0.95 (0.49) | 0.05 | 1 |
| Sweating or warm feeling before a spell | 1.95 (0.56) | <0.001 | 2 |
| Pre-syncope or syncope with pain or medical procedure | 2.90 (0.85) | <0.001 | 3 |
| . | Regression coefficient (SE) . | P-value . | Points . |
|---|---|---|---|
| Any one of bifascicular block, asystole, supraventricular tachycardia, diabetes | −4.93 (0.76) | <0.001 | −5 |
| Blue colour noted by bystander | −4.19 (1.26) | <0.001 | −4 |
| Age at first syncope ≥35 years | −2.61 (0.63) | <0.001 | −3 |
| Remembers something about the spell | −1.80 (0.53) | <0.001 | −2 |
| Pre-syncope or syncope with prolonged sitting or standing | 0.95 (0.49) | 0.05 | 1 |
| Sweating or warm feeling before a spell | 1.95 (0.56) | <0.001 | 2 |
| Pre-syncope or syncope with pain or medical procedure | 2.90 (0.85) | <0.001 | 3 |
Classify as tilt-positive primary syncope for points ≥−2.
Point scores for the diagnosis of tilt-positive primary syncope, in the absence of knowledge of the numbers and historical duration of syncope and pre-syncope
| . | Regression coefficient (SE) . | P-value . | Points . |
|---|---|---|---|
| Any one of bifascicular block, asystole, supraventricular tachycardia, diabetes | −4.93 (0.76) | <0.001 | −5 |
| Blue colour noted by bystander | −4.19 (1.26) | <0.001 | −4 |
| Age at first syncope ≥35 years | −2.61 (0.63) | <0.001 | −3 |
| Remembers something about the spell | −1.80 (0.53) | <0.001 | −2 |
| Pre-syncope or syncope with prolonged sitting or standing | 0.95 (0.49) | 0.05 | 1 |
| Sweating or warm feeling before a spell | 1.95 (0.56) | <0.001 | 2 |
| Pre-syncope or syncope with pain or medical procedure | 2.90 (0.85) | <0.001 | 3 |
| . | Regression coefficient (SE) . | P-value . | Points . |
|---|---|---|---|
| Any one of bifascicular block, asystole, supraventricular tachycardia, diabetes | −4.93 (0.76) | <0.001 | −5 |
| Blue colour noted by bystander | −4.19 (1.26) | <0.001 | −4 |
| Age at first syncope ≥35 years | −2.61 (0.63) | <0.001 | −3 |
| Remembers something about the spell | −1.80 (0.53) | <0.001 | −2 |
| Pre-syncope or syncope with prolonged sitting or standing | 0.95 (0.49) | 0.05 | 1 |
| Sweating or warm feeling before a spell | 1.95 (0.56) | <0.001 | 2 |
| Pre-syncope or syncope with pain or medical procedure | 2.90 (0.85) | <0.001 | 3 |
Classify as tilt-positive primary syncope for points ≥−2.
Diagnostic questions to determine whether syncope is due to vasovagal syncope or to another cause of syncope
| Question . | Points (if yes) . |
|---|---|
| Is there a history of at least one of bifascicular block, asystole, supraventricular tachycardia, diabetes? | −5 |
| At times have bystanders noted you to be blue during your faint? | −4 |
| Did your syncope start when you were 35 years of age or older? | −3 |
| Do you remember anything about being unconscious? | −2 |
| Do you have lightheaded spells or faint with prolonged sitting or standing? | 1 |
| Do you sweat or feel warm before a faint? | 2 |
| Do you have lightheaded spells or faint with pain or in medical settings? | 3 |
| Question . | Points (if yes) . |
|---|---|
| Is there a history of at least one of bifascicular block, asystole, supraventricular tachycardia, diabetes? | −5 |
| At times have bystanders noted you to be blue during your faint? | −4 |
| Did your syncope start when you were 35 years of age or older? | −3 |
| Do you remember anything about being unconscious? | −2 |
| Do you have lightheaded spells or faint with prolonged sitting or standing? | 1 |
| Do you sweat or feel warm before a faint? | 2 |
| Do you have lightheaded spells or faint with pain or in medical settings? | 3 |
The patient has vasovagal syncope if the point score is ≥−2.
Diagnostic questions to determine whether syncope is due to vasovagal syncope or to another cause of syncope
| Question . | Points (if yes) . |
|---|---|
| Is there a history of at least one of bifascicular block, asystole, supraventricular tachycardia, diabetes? | −5 |
| At times have bystanders noted you to be blue during your faint? | −4 |
| Did your syncope start when you were 35 years of age or older? | −3 |
| Do you remember anything about being unconscious? | −2 |
| Do you have lightheaded spells or faint with prolonged sitting or standing? | 1 |
| Do you sweat or feel warm before a faint? | 2 |
| Do you have lightheaded spells or faint with pain or in medical settings? | 3 |
| Question . | Points (if yes) . |
|---|---|
| Is there a history of at least one of bifascicular block, asystole, supraventricular tachycardia, diabetes? | −5 |
| At times have bystanders noted you to be blue during your faint? | −4 |
| Did your syncope start when you were 35 years of age or older? | −3 |
| Do you remember anything about being unconscious? | −2 |
| Do you have lightheaded spells or faint with prolonged sitting or standing? | 1 |
| Do you sweat or feel warm before a faint? | 2 |
| Do you have lightheaded spells or faint with pain or in medical settings? | 3 |
The patient has vasovagal syncope if the point score is ≥−2.
References
Hoefnagels WAJ, Padberg GW, Overweg J, Roos RAC. Syncope or seizure? A matter of opinion.
Kapoor WN, Karpf M, Wieand S, Peterson JR, Levey GS. A prospective evaluation and follow-up of patients with syncope.
Calkins H, Byrne M, El-Tassi R, Kalbfleisch S, Langberg JJ, Morady F. The economic burden of unrecognized vasodepressor syncope.
Sutton R, Petersen M. The economics of treating vasovagal syncope.
Linzer M, Yang EH, Estes III MA, Wang P, Vorperian VR, Kapoor W. Diagnosing Syncope. Part I. Value of history, physical examination, and electrocardiography.
Linzer M, Yang EH, Estes III MA, Wang P, Vorperian VR, Kapoor W. Diagnosing Syncope. Part II. Unexplained syncope.
Brignole M, Alboni P, Benditt DG, Bergfeldt L, Blanc JJ, Thomsen PE, Gert van Dijk J, Fitzpatrick A, Hohnloser S, Janousek J, Kapoor W, Kenny RA, Kulakowski P, Masotti G, Moya A, Raviele A, Sutton R, Theodorakis G, Ungar A, Wieling W, Priori SG, Garcia MA, Budaj A, Cowie M, Deckers J, Burgos EF, Lekakis J, Lindhal B, Mazzotta G, Morais J, Oto A, Smiseth O, Menozzi C, Ector H, Vardas P; Task Force on Syncope, European Society of Cardiology. Guidelines on management (diagnosis and treatment) of syncope-update 2004. Executive Summary.
Sheldon R, Rose S, Ritchie D, Connolly SJ, Koshman M, Lee MA, Frenneaux M, Fisher M, Murphy W. Historical criteria that distinguish syncope from seizures.
Sheldon R. Evaluation of a single-stage isoproterenol-tilt table test in patients with syncope.
Morillo CA, Klein GJ, Zandri S, Yee R. Diagnostic accuracy of a low-dose isoproterenol head-up tilt protocol.
Benditt DG, Ferguson DW, Grubb BP, Kapoor WN, Kugler J, Lerman BB, Maloney JD, Raviele A, Ross B, Sutton R, Wolk MJ, Wood DL. Tilt table testing for assessing syncope.
Fitzpatrick AP, Theodorakis G, Vardas P, Sutton R. Methodology of head-up tilt testing in patients with unexplained syncope.
Sheldon R, Killam S. Methodology of isoproterenol-tilt table testing in patients with syncope.
Sheldon RS, Rose S, Koshman ML. Isoproterenol tilt-table testing in patients with syncope and structural heart disease.
Grubb BP, Karas B. Clinical disorders of the autonomic nervous system associated with orthostatic intolerance. An overview of classification, clinical evaluation, and management.
Calkins H, Shyr Y, Frumin H, Schork A, Morady. The value of the clinical history in the differentiation of syncope due to ventricular tachycardia, atrioventricular block, and neurocardiogenic syncope.
Efron B. The Jacknife.
Van Donselaar CA, Geerts AT, Meulstee J, Habbema JDF, Staal A. Reliability of the diagnosis of a first seizure.
Alboni P, Brignole M, Menozzi C, Raviele A, Del Rosso A, Dinelli M Solano A, Bottoni N. Diagnostic value of history in patients with syncope with or without heart disease.
Sheldon R, Rose S, Koshman ML. Comparison of patients with syncope of unknown cause having negative or positive tilt-table tests.
Grimm W, Degenhardt M, Hoffman J, Menz V, Wirths A, Maisch B. Syncope recurrence can better be predicted by history than by head-up tilt testing in untreated patients with suspected neurally mediated syncope.
Moya A, Brignole M, Menozzi C, Garcia-Civera R, Tognarini S, Mont L, Botto G, Giada F, Cornacchia D. International Study on Syncope of Uncertain Etiology (ISSUE) Investigators. Mechanism of syncope in patients with isolated syncope and in patients with tilt-positive syncope.