-
PDF
- Split View
-
Views
-
Cite
Cite
Viktor Kočka, Martin Malý, Petr Toušek, Tomas Buděšínský, Libor Lisa, Petko Prodanov, Jiri Jarkovský, Petr Widimský, Bioresorbable vascular scaffolds in acute ST-segment elevation myocardial infarction: a prospective multicentre study ‘Prague 19’, European Heart Journal, Volume 35, Issue 12, 21 March 2014, Pages 787–794, https://doi.org/10.1093/eurheartj/eht545
Close - Share Icon Share
Abstract
Bioresorbable vascular scaffolds (BVSs) have been studied in chronic coronary artery disease, but not in acute ST-segment elevation myocardial infarction (STEMI). This prospective multicentre study analysed the feasibility and safety of BVS implantation during primary percutaneous coronary intervention (p-PCI) in STEMI.
Bioresorbable vascular scaffold implantation became the default strategy for all consecutive STEMI patients between 15 December 2012 and 30 August 2013. A total of 142 patients underwent p-PCI; 41 of them (28.9%) fulfilled the inclusion/exclusion criteria for BVS implantation. The BVS device success was 98%, thrombolysis in myocardial infarction 3 flow was restored in 95% of patients, and acute scaffold recoil was 9.7%. An optical coherence tomography (OCT) substudy (21 patients) demonstrated excellent procedural results with only a 1.1% rate of scaffold strut malapposition. Edge dissections were present in a 38% of patients, but were small and clinically silent. Reference vessel diameter measured by quantitative coronary angiography was significantly lower than that measured by OCT by 0.29 (±0.56) mm, P = 0.028. Clinical outcomes were compared between BVS group and Control group; the latter was formed by patients who had implanted metallic stent and were in Killip Class I or II. Combined clinical endpoint was defined as death, myocardial infarction, or target vessel revascularization. Event-free survival was the same in both groups; 95% for BVS and 93% for Control group, P = 0.674.
Bioresorbable vascular scaffold implantation in acute STEMI is feasible and safe. The procedural results evaluated by angiography and OCT are excellent. The early clinical results are encouraging.
See page 753 for the editorial comment on this article (doi:10.1093/eurheartj/ehu005)
Introduction
Everolimus-eluting stents have been shown to have favourable outcomes superior to the first generation of drug-eluting stents (DES),1 to be comparable with other second-generation DES2 and to be associated with a very low risk of stent thrombosis.3 Despite these excellent outcomes achieved with the modern DES, cardiologists and researchers continue their search for a fully bioresorbable stent. The first-in-human drug-eluting fully bioresorbable vascular scaffold (BVS) was implanted in 2006 in New Zealand.4 Since then, BVSs have been shown to be safe and effective in chronic stable coronary artery disease.5–8 The BVS use has not yet been systematically investigated in the highly thrombogenic setting of acute myocardial infarction with ST-segment elevation myocardial infarction (STEMI). The potential advantages of implanting BVS ( vs. other DES) in STEMI may be related to the fact that STEMI patients are frequently younger, have less extensive coronary artery disease (compared with non-STE acute coronary syndromes) and may live many years after successful primary percutaneous coronary intervention (p-PCI) and thus derive the benefit of not having a permanent rigid metallic structure in their coronary arteries.
The aim of this prospective multicentre open-labelled study was to analyse the feasibility and safety of BVS implanted during p-PCI. Besides describing the performance of BVS in acute STEMI and the outcomes of STEMI patients with BVS implantation, the study was also focused on the practical question—what proportion of consecutive STEMI patients are suitable candidates for the Absorb BVS implantation? The study is planned for 3 years, with a clinical follow-up plus CT coronary angiography after 1 year and invasive coronary angiography with optical coherence tomography (OCT) after 3 years. This study presents the procedural angiographic plus imaging results and early (up to 6 months) clinical outcomes.
Patients and methods
Study population
The protocol of this original academic prospective study was designed by the study authors and approved by the local ethical committee at each centre as well as by the national multicentric ethical committee. The study was conducted according to the Declaration of Helsinki, and written informed consent was obtained from all study patients. There was no support from industry; the cost of BVS was covered from institutional research funds. The study protocol prescribed to implant BVS (as a default strategy) to all consecutive STEMI patients who fulfilled the pre-specified inclusion and exclusion criteria (Table 1). All remaining patients were entered into a prospective registry. Dual antiplatelet therapy (DAPT) was recommended for 12 months (with a strict minimum of 6 months): a combination of prasugrel and aspirin was preferred but not mandated. All other aspects of acute and long-term care were standard and left at the discretion of the attending physicians.
Prague 19 study inclusion and exclusion criteria
| Inclusion criteria . | Exclusion criteria—clinical . | Exclusion criteria— angiographic . |
|---|---|---|
| STEMI <24 h from symptom onset | Killip III–IV class (high-likelihood of death within BVS resorbtion time) | Infarct artery reference diameter <2.3 or >3.7 mm (i.e. not suitable for currently available BVS sizes) |
| Signed written informed consent | Any other disease with probable prognosis <3 years | Lesion length >24 mm (i.e. precluding single BVS implantation) |
| Indication for oral anticoagulation (e.g. atrial fibrillation) | Extensive infarct artery calcifications or severe tortuosity | |
| Contraindication to prolonged dual antiplatelet therapy | STEMI caused by in-stent restenosis or stent thrombosis | |
| High-likelihood of non-compliance to DAPT | ||
| Inclusion criteria . | Exclusion criteria—clinical . | Exclusion criteria— angiographic . |
|---|---|---|
| STEMI <24 h from symptom onset | Killip III–IV class (high-likelihood of death within BVS resorbtion time) | Infarct artery reference diameter <2.3 or >3.7 mm (i.e. not suitable for currently available BVS sizes) |
| Signed written informed consent | Any other disease with probable prognosis <3 years | Lesion length >24 mm (i.e. precluding single BVS implantation) |
| Indication for oral anticoagulation (e.g. atrial fibrillation) | Extensive infarct artery calcifications or severe tortuosity | |
| Contraindication to prolonged dual antiplatelet therapy | STEMI caused by in-stent restenosis or stent thrombosis | |
| High-likelihood of non-compliance to DAPT | ||
Prague 19 study inclusion and exclusion criteria
| Inclusion criteria . | Exclusion criteria—clinical . | Exclusion criteria— angiographic . |
|---|---|---|
| STEMI <24 h from symptom onset | Killip III–IV class (high-likelihood of death within BVS resorbtion time) | Infarct artery reference diameter <2.3 or >3.7 mm (i.e. not suitable for currently available BVS sizes) |
| Signed written informed consent | Any other disease with probable prognosis <3 years | Lesion length >24 mm (i.e. precluding single BVS implantation) |
| Indication for oral anticoagulation (e.g. atrial fibrillation) | Extensive infarct artery calcifications or severe tortuosity | |
| Contraindication to prolonged dual antiplatelet therapy | STEMI caused by in-stent restenosis or stent thrombosis | |
| High-likelihood of non-compliance to DAPT | ||
| Inclusion criteria . | Exclusion criteria—clinical . | Exclusion criteria— angiographic . |
|---|---|---|
| STEMI <24 h from symptom onset | Killip III–IV class (high-likelihood of death within BVS resorbtion time) | Infarct artery reference diameter <2.3 or >3.7 mm (i.e. not suitable for currently available BVS sizes) |
| Signed written informed consent | Any other disease with probable prognosis <3 years | Lesion length >24 mm (i.e. precluding single BVS implantation) |
| Indication for oral anticoagulation (e.g. atrial fibrillation) | Extensive infarct artery calcifications or severe tortuosity | |
| Contraindication to prolonged dual antiplatelet therapy | STEMI caused by in-stent restenosis or stent thrombosis | |
| High-likelihood of non-compliance to DAPT | ||
Study device and procedure
The BVS 1.1 Absorb (Abbott Vascular, Santa Clara, CA, USA) balloon-expandable device consists of a polylactic acid polymer backbone processed for increased radial strength and a thin amorphous everolimus/polylactic acid matrix coating for controlled drug release. The implant is radiolucent, but two platinum markers at each end allow easy visualization on angiography. The single strut thickness is 150 µm. According to preclinical studies, the polymer backbone is fully absorbed in 2–3 years, and the polymer coating is absorbed faster.9
All patients received heparin anticoagulation, and GP IIbIIIa inhibitors use was left at the operator's discretion. Bioresorbable vascular scaffold implantation was preceded either by manual thrombus aspiration or by balloon pre-dilatation or both in all patients; balloon pre-dilatation was not mandatory but recommended. The inclusion criteria (maximal lesion length 24 mm) were selected to favour a single stent implantation. Bailout stenting of edge dissection detected by angiography or insufficient lesion coverage was performed with the study device if deemed safe by the operator. All operators were aware of the importance of avoiding or minimizing an overlap of BVS due to the significant thickness of stacked struts. Stent sizing was based on visual assessment by an experienced operator.
Quantitative coronary angiography and optical coherence tomography analysis
For each patient, quantitative coronary angiography (QCA) analysis was performed using the Philips Xcelera software. Intracoronary nitrates were administered to all normotensive patients. The last acquisition before BVS implantation was used for the analysis of interpolated reference vessel diameter (RVD) and maximal vessel diameter (Dmax) in the treated segment proximally and distally from stenosis. The images of the complete stent expansion (either by delivery balloon or by last post-dilatation balloon) and the cine frame immediately following in the same angiographic projection were used for acute device recoil measurement; mean diameters were compared.
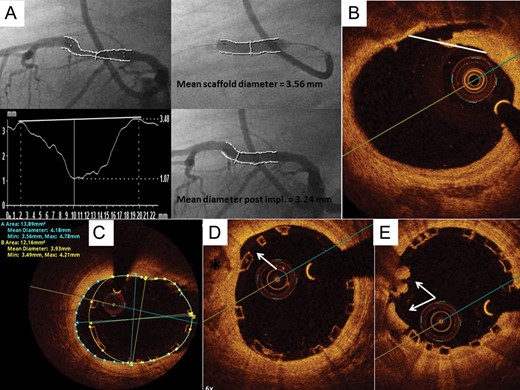
As an optional investigation, intracoronary OCT imaging using the frequency domain C7 system with a Dragonfly catheter (St. Jude Medical, St. Paul, MN, USA) was performed at the end of the procedure with a pullback speed of 20 mm per second and an image acquisition at 100 frames per second. The OCT measurements were performed with the proprietary software for offline analysis (St. Jude Medical); cross-sections were analysed at each 1 mm interval within the stented segment and 5 mm proximal and distal. Proximal and distal reference vessel area and mean diameter were measured at cross-section with a minimal disease within a 5 mm periscaffold segment. The analysis of BVS by OCT is different in comparison with metallic stents. The optically translucent polymeric struts appear as a black central core framed by light-scattering borders that do not shadow the vessel wall, thus allowing excellent visualization of the vessel wall behind the struts and evaluation of stent apposition. The main quantitative measurements evaluated were: scaffold area, mean diameter, and incomplete scaffold apposition (ISA) area. Both scaffold edges were examined for the presence of vessel dissection; if present, the size of the dissection was described as a percentage of lumen circumference. Edge dissection larger than 30% of lumen circumference was considered significant—we have opted for this simplified classification to enable quick visual assessment during p-PCI. Optical coherence tomography detected dissections tend to be small and clinical impact of minor edge dissection seems to be minimal.10 The presence and volume of thrombus were measured. Strut discontinuity was defined as the presence of two struts overhanging or an isolated strut in the centre of the vessel with no obvious connection to other struts. For QCA and OCT methodology see Figure 1, more detailed information on OCT methodology was published previously.11–14 Optical coherence tomography technology is not available in one of the participating centres (eight patients enrolled). An OCT investigation was left at the discretion of operator; however, patients with haemodynamic deterioration, ventricular arrhythmias, and large contrast load during p-PCI were generally not included.
Quantitative coronary angiography and optical coherence tomography measurements. (A) Quantitative coronary angiography measurements before bioresorbable vascular scaffold implantation, during balloon inflation and immediately post-implantation. Acute elastic recoil 9%. (B) Edge dissection by OCT, the maximal length of dissection is compared with artery circumference. (C) Moderately large incomplete scaffold apposition due to large vessel calibre at proximal scaffold edge. (D) Small incomplete scaffold apposition most likely due to vessel calcification (asterisk). (E) Small protruding thrombi, excellent scaffold apposition.
Endpoints and definitions
Baseline patient data for demographic characteristics, coronary angiography, and p-PCI (thrombolysis in myocardial infarction flow and residual stenosis) were collected. Device success was defined as the delivery and deployment of BVS at the intended target lesion with a final residual stenosis ≤20% by visual estimation. Bailout stenting was not considered as a device failure. The composite clinical endpoint was death, any myocardial infarction, and target vessel revascularization. Results are reported as per-treatment analysis.
Statistical analysis
Standard descriptive statistics were applied in the analysis: absolute and relative frequencies for categorical variables and mean supplemented by standard deviation for continuous variables. Statistical significance of differences between groups of patients was computed using Fisher's exact test for two category variables, maximum-likelihood χ2 test for category variables with more than two categories, and independent t-test for continuous variables. Paired t-test was used for the evaluation of statistical significance of differences between different measurements of vessel and scaffold diameter. Pearson and Spearman correlation coefficients were used for the analysis of the relationship between these measurements and Bland–Altman methodology for its visualization. Receiver operating characteristic (ROC) analysis was adopted for the analysis of potential predictors of vessel dissection and strut malapposition. The outcome of patients was described by means of Kaplan–Meier methodology, and statistical significance of differences in the combined clinical endpoint between groups of patients was tested using the log-rank test. The level of statistical significance was set at P = 0.05. IBM SPSS 21 for Windows (Release 21.0.0, IBM Corporation 2012) was used for data analysis.
Results
During the 8-month enrolment period from 15 December 2012 to 30 August 2013, 142 consecutive STEMI patients underwent emergent p-PCI and 49 BVS were used in 41 patients (29% of all consecutive STEMI patients). The analysis of exclusion criteria, i.e. the reasons why BVS could not be used in 71% of consecutive STEMI patients, are described in Table 2. The BVS device success rate was 98% (40 of 41 patients) without any technical difficulties. In one patient with left circumflex coronary artery occlusion, BVS could not pass through the angulated left circumflex (LCX) take-off and a bare metal stent was implanted instead; this patient was further evaluated within the Control group. The clinical outcomes were analysed in two pre-specified groups: (i) BVS group (n = 40, according to exclusion criteria all patients in Killip I–II class) and (ii) Control group (drug-eluting or bare metal stent implanted in Killip I–II class patients; n = 57). The remaining 45 patients (24 STEMI patients presenting with severe acute heart failure, i.e. Killip III–IV and 21 STEMI patients without stent implantation) were not used for this comparison purpose, but baseline characteristics are described in the article in order to provide a full picture of non-selected consecutive STEMI series and to put BVS use into proper perspective within a real-life STEMI scenario. The baseline characteristics of all the three groups are provided in Table 3. Primary percutaneous coronary intervention femoral access dominated in both groups with the radial route used in eight patients in both groups. Bailout stenting for edge dissection was performed in three patients. Procedural details of p-PCI are summarized in Table 4.
Analysis of Prague 19 study exclusion criteria (n = 101 patients excluded from receiving bioresorbable vascular scaffold)
| Exclusion criteria . | No. of patients . |
|---|---|
| Clinical—total | 44 |
| Killip III–IV | 24 |
| Stent thrombosis | 5 |
| Poor compliance | 8 |
| Comorbidity with limited expected survival | 3 |
| Anticoagulation or contraindication of DAPT | 4 |
| Technical—total | 51 |
| Vessel diameter outside 2.3–3.7 mm range | 30 |
| Correct BVS size not in stock | 14 |
| Vessel calcification/tortuosity | 17 |
| p-PCI without stent implantation | 21 |
| Exclusion criteria . | No. of patients . |
|---|---|
| Clinical—total | 44 |
| Killip III–IV | 24 |
| Stent thrombosis | 5 |
| Poor compliance | 8 |
| Comorbidity with limited expected survival | 3 |
| Anticoagulation or contraindication of DAPT | 4 |
| Technical—total | 51 |
| Vessel diameter outside 2.3–3.7 mm range | 30 |
| Correct BVS size not in stock | 14 |
| Vessel calcification/tortuosity | 17 |
| p-PCI without stent implantation | 21 |
Patients could have multiple exclusion criteria.
DAPT, dual antiplatelet therapy; BVS, bioresorbable vascular scaffold; p-PCI, primary percutaneous coronary intervention.
Analysis of Prague 19 study exclusion criteria (n = 101 patients excluded from receiving bioresorbable vascular scaffold)
| Exclusion criteria . | No. of patients . |
|---|---|
| Clinical—total | 44 |
| Killip III–IV | 24 |
| Stent thrombosis | 5 |
| Poor compliance | 8 |
| Comorbidity with limited expected survival | 3 |
| Anticoagulation or contraindication of DAPT | 4 |
| Technical—total | 51 |
| Vessel diameter outside 2.3–3.7 mm range | 30 |
| Correct BVS size not in stock | 14 |
| Vessel calcification/tortuosity | 17 |
| p-PCI without stent implantation | 21 |
| Exclusion criteria . | No. of patients . |
|---|---|
| Clinical—total | 44 |
| Killip III–IV | 24 |
| Stent thrombosis | 5 |
| Poor compliance | 8 |
| Comorbidity with limited expected survival | 3 |
| Anticoagulation or contraindication of DAPT | 4 |
| Technical—total | 51 |
| Vessel diameter outside 2.3–3.7 mm range | 30 |
| Correct BVS size not in stock | 14 |
| Vessel calcification/tortuosity | 17 |
| p-PCI without stent implantation | 21 |
Patients could have multiple exclusion criteria.
DAPT, dual antiplatelet therapy; BVS, bioresorbable vascular scaffold; p-PCI, primary percutaneous coronary intervention.
Baseline characteristics
| . | Killip III–IV or no-stent group (N = 45), n (%)/mean (SD) . | BVS groupa (N = 40), n (%)/mean (SD) . | Control groupa (N = 57), n (%)/mean (SD) . | P-valuea . |
|---|---|---|---|---|
| Male | 25 (55.5%) | 31 (77.5%) | 43 (75.4%) | 1.000 |
| Age | 69.0 (13.3) | 58.9 (10.9) | 63.8 (12.9) | 0.735 |
| Mean Killip class | 2.45 (1.26) | 1.08 (0.27) | 1.12 (0.33) | 0.460 |
| Diabetes mellitus | 14 (31.1%) | 1 (2.5%) | 14 (24.6%) | 0.003 |
| Current smoking | 27 (60.0%) | 25 (62.5%) | 33 (57.9%) | 0.671 |
| Prior myocardial infarction | 7 (15.6%) | 1 (2.5%) | 7 (12.3%) | 0.137 |
| Prior PCI | 10 (22.2%) | 1 (2.5%) | 5 (8.8%) | 0.396 |
| Prior CABG | 1 (2.2%) | 0 (0.0%) | 1 (1.8%) | 1.000 |
| LAD infarct | 22 (48.9%) | 20 (50.0%) | 19 (33.3%) | 0.093 |
| LCX infarct | 7 (15.6%) | 11 (27.5%) | 11 (19.3%) | 0.465 |
| RCA infarct | 16 (35.6%) | 9 (22.5%) | 27 (47.3%) | 0.011 |
| . | Killip III–IV or no-stent group (N = 45), n (%)/mean (SD) . | BVS groupa (N = 40), n (%)/mean (SD) . | Control groupa (N = 57), n (%)/mean (SD) . | P-valuea . |
|---|---|---|---|---|
| Male | 25 (55.5%) | 31 (77.5%) | 43 (75.4%) | 1.000 |
| Age | 69.0 (13.3) | 58.9 (10.9) | 63.8 (12.9) | 0.735 |
| Mean Killip class | 2.45 (1.26) | 1.08 (0.27) | 1.12 (0.33) | 0.460 |
| Diabetes mellitus | 14 (31.1%) | 1 (2.5%) | 14 (24.6%) | 0.003 |
| Current smoking | 27 (60.0%) | 25 (62.5%) | 33 (57.9%) | 0.671 |
| Prior myocardial infarction | 7 (15.6%) | 1 (2.5%) | 7 (12.3%) | 0.137 |
| Prior PCI | 10 (22.2%) | 1 (2.5%) | 5 (8.8%) | 0.396 |
| Prior CABG | 1 (2.2%) | 0 (0.0%) | 1 (1.8%) | 1.000 |
| LAD infarct | 22 (48.9%) | 20 (50.0%) | 19 (33.3%) | 0.093 |
| LCX infarct | 7 (15.6%) | 11 (27.5%) | 11 (19.3%) | 0.465 |
| RCA infarct | 16 (35.6%) | 9 (22.5%) | 27 (47.3%) | 0.011 |
CABG, coronary artery bypass grafting; LAD, left anterior descending; LCX, left circumflex; RCA, right coronary artery. Bold are significant (P < 0.05).
aStatistical significance of differences between bioresorbable vascular scaffold and Control groups tested by Fisher's exact test for two category variables, by the maximum-likelihood χ2 test for categorical variables with more than two categories and by the independent t-test for continuous variables.
Baseline characteristics
| . | Killip III–IV or no-stent group (N = 45), n (%)/mean (SD) . | BVS groupa (N = 40), n (%)/mean (SD) . | Control groupa (N = 57), n (%)/mean (SD) . | P-valuea . |
|---|---|---|---|---|
| Male | 25 (55.5%) | 31 (77.5%) | 43 (75.4%) | 1.000 |
| Age | 69.0 (13.3) | 58.9 (10.9) | 63.8 (12.9) | 0.735 |
| Mean Killip class | 2.45 (1.26) | 1.08 (0.27) | 1.12 (0.33) | 0.460 |
| Diabetes mellitus | 14 (31.1%) | 1 (2.5%) | 14 (24.6%) | 0.003 |
| Current smoking | 27 (60.0%) | 25 (62.5%) | 33 (57.9%) | 0.671 |
| Prior myocardial infarction | 7 (15.6%) | 1 (2.5%) | 7 (12.3%) | 0.137 |
| Prior PCI | 10 (22.2%) | 1 (2.5%) | 5 (8.8%) | 0.396 |
| Prior CABG | 1 (2.2%) | 0 (0.0%) | 1 (1.8%) | 1.000 |
| LAD infarct | 22 (48.9%) | 20 (50.0%) | 19 (33.3%) | 0.093 |
| LCX infarct | 7 (15.6%) | 11 (27.5%) | 11 (19.3%) | 0.465 |
| RCA infarct | 16 (35.6%) | 9 (22.5%) | 27 (47.3%) | 0.011 |
| . | Killip III–IV or no-stent group (N = 45), n (%)/mean (SD) . | BVS groupa (N = 40), n (%)/mean (SD) . | Control groupa (N = 57), n (%)/mean (SD) . | P-valuea . |
|---|---|---|---|---|
| Male | 25 (55.5%) | 31 (77.5%) | 43 (75.4%) | 1.000 |
| Age | 69.0 (13.3) | 58.9 (10.9) | 63.8 (12.9) | 0.735 |
| Mean Killip class | 2.45 (1.26) | 1.08 (0.27) | 1.12 (0.33) | 0.460 |
| Diabetes mellitus | 14 (31.1%) | 1 (2.5%) | 14 (24.6%) | 0.003 |
| Current smoking | 27 (60.0%) | 25 (62.5%) | 33 (57.9%) | 0.671 |
| Prior myocardial infarction | 7 (15.6%) | 1 (2.5%) | 7 (12.3%) | 0.137 |
| Prior PCI | 10 (22.2%) | 1 (2.5%) | 5 (8.8%) | 0.396 |
| Prior CABG | 1 (2.2%) | 0 (0.0%) | 1 (1.8%) | 1.000 |
| LAD infarct | 22 (48.9%) | 20 (50.0%) | 19 (33.3%) | 0.093 |
| LCX infarct | 7 (15.6%) | 11 (27.5%) | 11 (19.3%) | 0.465 |
| RCA infarct | 16 (35.6%) | 9 (22.5%) | 27 (47.3%) | 0.011 |
CABG, coronary artery bypass grafting; LAD, left anterior descending; LCX, left circumflex; RCA, right coronary artery. Bold are significant (P < 0.05).
aStatistical significance of differences between bioresorbable vascular scaffold and Control groups tested by Fisher's exact test for two category variables, by the maximum-likelihood χ2 test for categorical variables with more than two categories and by the independent t-test for continuous variables.
Primary PCI data
| . | BVS group (N = 40), n (%)/mean (SD) . | Control group (N = 57), n (%)/mean (SD) . | P-value* . |
|---|---|---|---|
| Door to reperfusion (min) | 29.9 (10.0) | 27.7 (9.2) | 0.284 |
| Manual aspiration thrombectomy | 15 (37.5%) | 7 (12.3%) | 0.011 |
| Pre-dilatation | 34 (85.0%) | 46 (80.7%) | 0.578 |
| Pre-dilatation balloon undersizing (mm)a | 0.7 (0.4) | 1.0 (0.7) | 0.005 |
| Post-dilatation | 13 (32.5%) | 18 (31.6%) | 1.000 |
| Max. atm. | 15.4 (2.1) | 15.3 (1.2) | 0.934 |
| Mean no. of scaffolds/stents | 1.2 | 1.28 | 0.760 |
| Scaffold/stent size (mm) | 3.3 (0.3) | 3.6 (0.5) | 0.006 |
| Total scaffold/stent length (mm) | 23.2 (10.4) | 24.1 (13.0) | 0.706 |
| Diameter stenosis pre | |||
| <100% | 18 (45.0%) | 24 (42.1%) | 0.834 |
| 100% | 22 (55.0%) | 33 (57.9%) | |
| Diameter stenosis post | |||
| ≤20% | 40 (100.0%) | 54 (94.7%) | 0.269 |
| >20% | 0 (0.0%) | 3 (5.3%) | |
| TIMI flow pre | |||
| 0 | 22 (55.5%) | 34 (59.6%) | 0.382 |
| 1 | 2 (5.0%) | 1 (1.8%) | |
| 2 | 11 (27.5%) | 10 (17.5%) | |
| 3 | 5 (12.5%) | 12 (21.1%) | |
| TIMI flow post | |||
| 0 | 0 (0.0%) | 2 (3.5%) | 0.521 |
| 1 | 1 (2.5%) | 1 (1.8%) | |
| 2 | 1 (2.5%) | 2 (3.5%) | |
| 3 | 38 (95.0%) | 52 (91.2%) | |
| Troponin T (ng/L) maxb | 3 581.1 (2 925.4) | 3 571.1 (3 002.6) | 0.672 |
| . | BVS group (N = 40), n (%)/mean (SD) . | Control group (N = 57), n (%)/mean (SD) . | P-value* . |
|---|---|---|---|
| Door to reperfusion (min) | 29.9 (10.0) | 27.7 (9.2) | 0.284 |
| Manual aspiration thrombectomy | 15 (37.5%) | 7 (12.3%) | 0.011 |
| Pre-dilatation | 34 (85.0%) | 46 (80.7%) | 0.578 |
| Pre-dilatation balloon undersizing (mm)a | 0.7 (0.4) | 1.0 (0.7) | 0.005 |
| Post-dilatation | 13 (32.5%) | 18 (31.6%) | 1.000 |
| Max. atm. | 15.4 (2.1) | 15.3 (1.2) | 0.934 |
| Mean no. of scaffolds/stents | 1.2 | 1.28 | 0.760 |
| Scaffold/stent size (mm) | 3.3 (0.3) | 3.6 (0.5) | 0.006 |
| Total scaffold/stent length (mm) | 23.2 (10.4) | 24.1 (13.0) | 0.706 |
| Diameter stenosis pre | |||
| <100% | 18 (45.0%) | 24 (42.1%) | 0.834 |
| 100% | 22 (55.0%) | 33 (57.9%) | |
| Diameter stenosis post | |||
| ≤20% | 40 (100.0%) | 54 (94.7%) | 0.269 |
| >20% | 0 (0.0%) | 3 (5.3%) | |
| TIMI flow pre | |||
| 0 | 22 (55.5%) | 34 (59.6%) | 0.382 |
| 1 | 2 (5.0%) | 1 (1.8%) | |
| 2 | 11 (27.5%) | 10 (17.5%) | |
| 3 | 5 (12.5%) | 12 (21.1%) | |
| TIMI flow post | |||
| 0 | 0 (0.0%) | 2 (3.5%) | 0.521 |
| 1 | 1 (2.5%) | 1 (1.8%) | |
| 2 | 1 (2.5%) | 2 (3.5%) | |
| 3 | 38 (95.0%) | 52 (91.2%) | |
| Troponin T (ng/L) maxb | 3 581.1 (2 925.4) | 3 571.1 (3 002.6) | 0.672 |
aPatients with pre-dilatation only.
bStatistical significance of difference was calculated on logarithmically transformed data (LN(x)).
*Statistical significance of differences between groups tested by Fisher's exact test for two category variables, by the ML χ2 test for categorical variables with more than two categories and by the independent t-test for continuous variables.
Bold are significant (P < 0.05).
Primary PCI data
| . | BVS group (N = 40), n (%)/mean (SD) . | Control group (N = 57), n (%)/mean (SD) . | P-value* . |
|---|---|---|---|
| Door to reperfusion (min) | 29.9 (10.0) | 27.7 (9.2) | 0.284 |
| Manual aspiration thrombectomy | 15 (37.5%) | 7 (12.3%) | 0.011 |
| Pre-dilatation | 34 (85.0%) | 46 (80.7%) | 0.578 |
| Pre-dilatation balloon undersizing (mm)a | 0.7 (0.4) | 1.0 (0.7) | 0.005 |
| Post-dilatation | 13 (32.5%) | 18 (31.6%) | 1.000 |
| Max. atm. | 15.4 (2.1) | 15.3 (1.2) | 0.934 |
| Mean no. of scaffolds/stents | 1.2 | 1.28 | 0.760 |
| Scaffold/stent size (mm) | 3.3 (0.3) | 3.6 (0.5) | 0.006 |
| Total scaffold/stent length (mm) | 23.2 (10.4) | 24.1 (13.0) | 0.706 |
| Diameter stenosis pre | |||
| <100% | 18 (45.0%) | 24 (42.1%) | 0.834 |
| 100% | 22 (55.0%) | 33 (57.9%) | |
| Diameter stenosis post | |||
| ≤20% | 40 (100.0%) | 54 (94.7%) | 0.269 |
| >20% | 0 (0.0%) | 3 (5.3%) | |
| TIMI flow pre | |||
| 0 | 22 (55.5%) | 34 (59.6%) | 0.382 |
| 1 | 2 (5.0%) | 1 (1.8%) | |
| 2 | 11 (27.5%) | 10 (17.5%) | |
| 3 | 5 (12.5%) | 12 (21.1%) | |
| TIMI flow post | |||
| 0 | 0 (0.0%) | 2 (3.5%) | 0.521 |
| 1 | 1 (2.5%) | 1 (1.8%) | |
| 2 | 1 (2.5%) | 2 (3.5%) | |
| 3 | 38 (95.0%) | 52 (91.2%) | |
| Troponin T (ng/L) maxb | 3 581.1 (2 925.4) | 3 571.1 (3 002.6) | 0.672 |
| . | BVS group (N = 40), n (%)/mean (SD) . | Control group (N = 57), n (%)/mean (SD) . | P-value* . |
|---|---|---|---|
| Door to reperfusion (min) | 29.9 (10.0) | 27.7 (9.2) | 0.284 |
| Manual aspiration thrombectomy | 15 (37.5%) | 7 (12.3%) | 0.011 |
| Pre-dilatation | 34 (85.0%) | 46 (80.7%) | 0.578 |
| Pre-dilatation balloon undersizing (mm)a | 0.7 (0.4) | 1.0 (0.7) | 0.005 |
| Post-dilatation | 13 (32.5%) | 18 (31.6%) | 1.000 |
| Max. atm. | 15.4 (2.1) | 15.3 (1.2) | 0.934 |
| Mean no. of scaffolds/stents | 1.2 | 1.28 | 0.760 |
| Scaffold/stent size (mm) | 3.3 (0.3) | 3.6 (0.5) | 0.006 |
| Total scaffold/stent length (mm) | 23.2 (10.4) | 24.1 (13.0) | 0.706 |
| Diameter stenosis pre | |||
| <100% | 18 (45.0%) | 24 (42.1%) | 0.834 |
| 100% | 22 (55.0%) | 33 (57.9%) | |
| Diameter stenosis post | |||
| ≤20% | 40 (100.0%) | 54 (94.7%) | 0.269 |
| >20% | 0 (0.0%) | 3 (5.3%) | |
| TIMI flow pre | |||
| 0 | 22 (55.5%) | 34 (59.6%) | 0.382 |
| 1 | 2 (5.0%) | 1 (1.8%) | |
| 2 | 11 (27.5%) | 10 (17.5%) | |
| 3 | 5 (12.5%) | 12 (21.1%) | |
| TIMI flow post | |||
| 0 | 0 (0.0%) | 2 (3.5%) | 0.521 |
| 1 | 1 (2.5%) | 1 (1.8%) | |
| 2 | 1 (2.5%) | 2 (3.5%) | |
| 3 | 38 (95.0%) | 52 (91.2%) | |
| Troponin T (ng/L) maxb | 3 581.1 (2 925.4) | 3 571.1 (3 002.6) | 0.672 |
aPatients with pre-dilatation only.
bStatistical significance of difference was calculated on logarithmically transformed data (LN(x)).
*Statistical significance of differences between groups tested by Fisher's exact test for two category variables, by the ML χ2 test for categorical variables with more than two categories and by the independent t-test for continuous variables.
Bold are significant (P < 0.05).
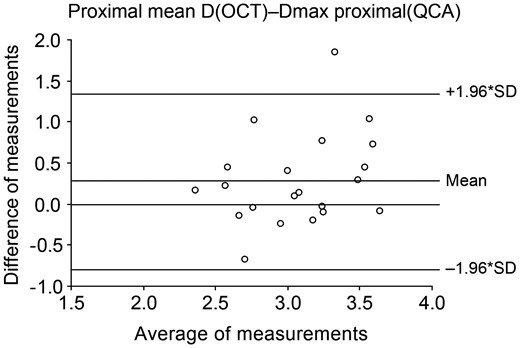
Twenty-one patients had OCT intracoronary imaging performed at the end of p-PCI without any complication. A visual estimate of scaffold apposition and edge dissection was performed by the operator, with recommendation to consider the treatment of edge dissections larger than 30% of lumen circumference and to consider post-dilatation in the case of malapposition detectable in multiple frames; no such cases were, however, encountered. Post hoc QCA and OCT analyses were performed and results are presented in Table 5. There are significant differences between QCA and OCT measurements. The proximal reference diameter measured by OCT is larger by 0.29 (±0.56) mm than Dmax proximal measured by QCA, P = 0.028 (Figure 2). The scaffold-to-artery ratio based on QCA/OCT is 1.26/1.14 indicating a significant oversizing, and OCT derived scaffold oversize (defined as ideal scaffold diameter at implantation pressure minus proximal reference diameter by OCT) is a significant negative predictor of strut malapposition; area under the curve (95% confidence interval) = 0.77 (0.56; 0.99), P = 0.035, based on ROC analysis. Scaffold oversize measured by either OCT or QCA did not predict the occurrence of edge dissection. There was no strut discontinuity detected.
QCA and OCT substudy results (n = 21 patients, 432 frames and 4329 struts)
| Parameter . | n (%)/mean (SD) . |
|---|---|
| Ideal scaffold diameter at implantation pressure as per chart, mm | 3.68 (0.40) |
| QCA analysis | |
| Interpolated RVD, mm | 2.80 (0.38) |
| Dmax proximal/distal, mm | 2.93 (0.40)/2.72 (0.40) |
| Mean scaffold diameter during deployment, mm | 3.08 (0.39) |
| Mean vessel diameter immediately post-BVS implantation, mm | 2.78 (0.29) |
| Acute recoil, mm (%) | 0.30 (9.7%) |
| OCT analysis at the end of p-PCI | |
| Proximal reference diameter, mm | 3.22 (0.53) |
| Distal reference diameter, mm | 2.81 (0.49) |
| Mean scaffold area, mm2 | 8.19 (1.50) |
| Mean scaffold diameter, mm | 3.20 (0.31) |
| Mean lumen area, mm2 | 7.71 (1.43) |
| Mean lumen diamater, mm | 3.12 (0.28) |
| Thrombus detected (% of patients/% of frames) | 20 (95%)/4 (19%) |
| Malapposition detected (% of patients/% of struts) | 10 (47.6%)/47 (1.1%) |
| ISA area, mm2 | 0.11 (0.21) |
| Significant malapposition (>5% of struts per patient) | 0 (0%) |
| Edge dissection detected (proximal or distal; % of patients) | 8 (38%) |
| Edge dissection mean size (% of scaffold circumference) | 15.8% |
| Parameter . | n (%)/mean (SD) . |
|---|---|
| Ideal scaffold diameter at implantation pressure as per chart, mm | 3.68 (0.40) |
| QCA analysis | |
| Interpolated RVD, mm | 2.80 (0.38) |
| Dmax proximal/distal, mm | 2.93 (0.40)/2.72 (0.40) |
| Mean scaffold diameter during deployment, mm | 3.08 (0.39) |
| Mean vessel diameter immediately post-BVS implantation, mm | 2.78 (0.29) |
| Acute recoil, mm (%) | 0.30 (9.7%) |
| OCT analysis at the end of p-PCI | |
| Proximal reference diameter, mm | 3.22 (0.53) |
| Distal reference diameter, mm | 2.81 (0.49) |
| Mean scaffold area, mm2 | 8.19 (1.50) |
| Mean scaffold diameter, mm | 3.20 (0.31) |
| Mean lumen area, mm2 | 7.71 (1.43) |
| Mean lumen diamater, mm | 3.12 (0.28) |
| Thrombus detected (% of patients/% of frames) | 20 (95%)/4 (19%) |
| Malapposition detected (% of patients/% of struts) | 10 (47.6%)/47 (1.1%) |
| ISA area, mm2 | 0.11 (0.21) |
| Significant malapposition (>5% of struts per patient) | 0 (0%) |
| Edge dissection detected (proximal or distal; % of patients) | 8 (38%) |
| Edge dissection mean size (% of scaffold circumference) | 15.8% |
QCA and OCT substudy results (n = 21 patients, 432 frames and 4329 struts)
| Parameter . | n (%)/mean (SD) . |
|---|---|
| Ideal scaffold diameter at implantation pressure as per chart, mm | 3.68 (0.40) |
| QCA analysis | |
| Interpolated RVD, mm | 2.80 (0.38) |
| Dmax proximal/distal, mm | 2.93 (0.40)/2.72 (0.40) |
| Mean scaffold diameter during deployment, mm | 3.08 (0.39) |
| Mean vessel diameter immediately post-BVS implantation, mm | 2.78 (0.29) |
| Acute recoil, mm (%) | 0.30 (9.7%) |
| OCT analysis at the end of p-PCI | |
| Proximal reference diameter, mm | 3.22 (0.53) |
| Distal reference diameter, mm | 2.81 (0.49) |
| Mean scaffold area, mm2 | 8.19 (1.50) |
| Mean scaffold diameter, mm | 3.20 (0.31) |
| Mean lumen area, mm2 | 7.71 (1.43) |
| Mean lumen diamater, mm | 3.12 (0.28) |
| Thrombus detected (% of patients/% of frames) | 20 (95%)/4 (19%) |
| Malapposition detected (% of patients/% of struts) | 10 (47.6%)/47 (1.1%) |
| ISA area, mm2 | 0.11 (0.21) |
| Significant malapposition (>5% of struts per patient) | 0 (0%) |
| Edge dissection detected (proximal or distal; % of patients) | 8 (38%) |
| Edge dissection mean size (% of scaffold circumference) | 15.8% |
| Parameter . | n (%)/mean (SD) . |
|---|---|
| Ideal scaffold diameter at implantation pressure as per chart, mm | 3.68 (0.40) |
| QCA analysis | |
| Interpolated RVD, mm | 2.80 (0.38) |
| Dmax proximal/distal, mm | 2.93 (0.40)/2.72 (0.40) |
| Mean scaffold diameter during deployment, mm | 3.08 (0.39) |
| Mean vessel diameter immediately post-BVS implantation, mm | 2.78 (0.29) |
| Acute recoil, mm (%) | 0.30 (9.7%) |
| OCT analysis at the end of p-PCI | |
| Proximal reference diameter, mm | 3.22 (0.53) |
| Distal reference diameter, mm | 2.81 (0.49) |
| Mean scaffold area, mm2 | 8.19 (1.50) |
| Mean scaffold diameter, mm | 3.20 (0.31) |
| Mean lumen area, mm2 | 7.71 (1.43) |
| Mean lumen diamater, mm | 3.12 (0.28) |
| Thrombus detected (% of patients/% of frames) | 20 (95%)/4 (19%) |
| Malapposition detected (% of patients/% of struts) | 10 (47.6%)/47 (1.1%) |
| ISA area, mm2 | 0.11 (0.21) |
| Significant malapposition (>5% of struts per patient) | 0 (0%) |
| Edge dissection detected (proximal or distal; % of patients) | 8 (38%) |
| Edge dissection mean size (% of scaffold circumference) | 15.8% |
Bland–Altman plots for the measurement comparison of proximal segment reference diameter measured by OCT and QCA, and OCT measured diameter is larger by 0.29 (±0.56) mm, P = 0.028.
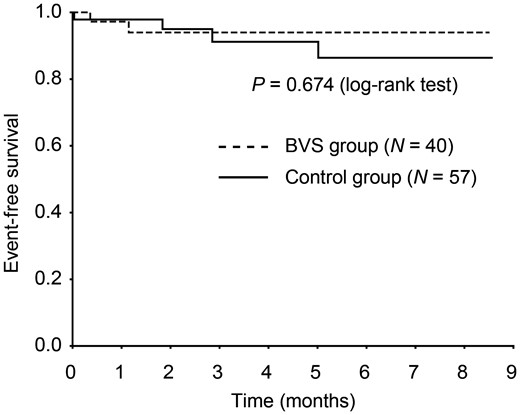
Clinical results are summarized in Figure 3. We have achieved a 100% follow-up in the BVS group and 96.5% in the Control group—two patients (both temporary Prague visitors from abroad) were not reached. There were two events in the BVS group and four in the Control group. One patient with two BVS implanted in his left anterior descending (LAD) suffered scaffold thrombosis on Day 13, 3 days after he stopped using all prescribed medication including ticagrelor and aspirin. He was treated with repeat p-PCI in March 2013 with balloon dilatation only, has excellent compliance with medication since this event, and his further course is uneventful. The second patient with three BVS implanted to his LAD underwent planned staged PCI of his LCX coronary artery with drug-eluting metallic stent 5 weeks after p-PCI and had a small myocardial infarction due to side branch occlusion. This was completely unrelated to the previously implanted BVS, but fulfilled the pre-specified criteria of any myocardial infarction. With regard to the Control group, one patient died of cardiogenic shock on Day 2; two patients presented with unstable angina due to stent restenosis (one bare metal and one DES) and were treated with surgical revascularization; and the fourth patient with index p-PCI to his LAD suffered from non-ST-elevation myocardial infarction with culprit lesion in the LCX.
Kaplan–Meier event curves comparing bioresorbable vascular scaffold and Control group for a composite endpoint of cardiac death, any myocardial infarction, and target vessel revascularization. The number of patients available for follow-up in the bioresorbable vascular scaffold/Control group is 40/57 at discharge, 36/48 at 1 month, and 17/25 at 6 months.
Discussion
The study results showed that BVS implantation in STEMI patients is feasible and initial estimates of safety are satisfactory. The potential advantages of bioresorbable scaffold in this setting are further discussed below.
How many patients with STEMI could potentially be treated with bioresorbable scaffolds?
Complete bioresorption (the mechanism of potential benefit) takes at least 2 years after implantation based on preclinical studies.9 Thus, we did not consider BVS in patients with uncertain prognosis over this time span. The other important clinical exclusion was the potential issue with 12 months DAPT. Only 3.23% of struts were previously found uncovered by OCT at 6 months post-implantation,12 and the published design of ABSORB II randomized trial15 mandates only 6 months DAPT duration. Positive results of this trial could make the issue of DAPT after BVS Absorb implantation less important. From the technical perspective, the production of larger (at least 4.0 mm diameter), longer, and smaller profile scaffolds would significantly increase the proportion of STEMI patients suitable for BVS implantation. The issue of very short expiration time with resulting problems of BVS stocking will surely be addressed.
Scaffold mechanical properties and procedural results
An objective comparison with metallic stents (Multilink Vision) and DES (Xience) found that BVS have better conformability than conventional stents after implantation.16 However, due to thicker struts and crossing profile, the pushability of the device is worse than second-generation DES; despite careful exclusion of heavily calcified or tortuous arteries we failed to deploy BVS in one patient with a sharp angled take-off of otherwise non-calcified and non-tortuous left circumflex artery. Despite large scaffold-to-artery ratio, the acute recoil is very similar to the previously published data on stable patients.17 The edge dissections detected by OCT were relatively frequent, but small, not detectable by angiography and in all our cases clinically silent. The significant stent oversizing has most likely helped us to achieve an excellent acute result with regard to scaffold strut malapposition, and only 1.1% of struts were malapposed when compared with 3.5% of malapposed struts in the OCT substudy of ABSORB Cohort B.14 The issue of correct scaffold sizing is crucial and the statistically significant difference between the measurement of proximal reference diameter by QCA and OCT is very relevant, the difference was larger than 0.5 mm in 5 of 21 patients evaluated. Online QCA has been incorporated into the ABSORB II randomized trial design,15 but based on our results this would lead to significant scaffold undersizing.
Thrombus containing lesions and bioresorbable vascular scaffold
The published studies with BVS in chronic stable patients demonstrated a very low risk of stent thrombosis or restenosis. It is not known whether BVSs are similarly safe in patients with STEMI—the most prothrombotic condition among all forms of atherosclerosis. All treated lesions had angiographic evidence of thrombus before p-PCI. The optical coherence tomography evidence of thrombus still present at the end of p-PCI in 20 of 21 studied patients. There was one case of subacute scaffold thrombosis due to patient discontinuation of DAPT. This patient had a second BVS implanted due to angiographically evident distal edge dissection during the index p-PCI; final result was optimal. He did not have OCT performed at the baseline due to ventricular arrhythmias requiring defibrillation four times. During repeat p-PCI on Day 13, the manual aspiration thrombectomy was followed by OCT, which demonstrated a 2 mm gap between scaffolds as a possible minor contributing factor. This region was post-dilated and left without further intervention. Stacked overlapping BVS struts with a minimum thickness of 300 µm could present a risk of delayed endothelialization18 and are best avoided. Our study is planned for 3-year follow-up to confirm also the long-term safety.
Study limitations
As far as clinical outcomes are concerned, the small number of patients and selection bias due to inclusion/exclusion criteria does not allow us to reach definitive conclusions. Rather, we present initial findings from an ongoing study and some variation in the clinical results once all data is accumulated could be expected. However, our OCT and QCA data are robust.
Thus, this study results showed that BVS implantation in acute STEMI is feasible and safe and could be potentially used in a larger proportion of patients. The strategy of significant scaffold oversizing in the setting of primary PCI results in excellent acute procedural results. A very low rate of strut malapposition was demonstrated by OCT. The short-term clinical outcomes are encouraging, but will require a longer follow-up.
Funding
The study was funded from the research project no. PRVOUK P35, Charles University, Prague. Funding to pay the Open Access publication charges for this article was provided by research project no. PRVOUK P35, Charles University, Prague.
Conflict of interest: This study was not supported by industry and none of the authors received any renumeration for their participation in this study. V.K. and P.W. received occasional speaker honoraria from Abbott Vascular.
Acknowledgements
We thank Radka Tichá for her help with Prague 19 study database.