-
PDF
- Split View
-
Views
-
Cite
Cite
Nicola Ryan, Javier Escaned, Myocardial bridge as a cause of persistent post percutaneous coronary intervention angina identified with exercise intracoronary physiology, European Heart Journal, Volume 38, Issue 13, 1 April 2017, Page 1001, https://doi.org/10.1093/eurheartj/ehw501
Close - Share Icon Share
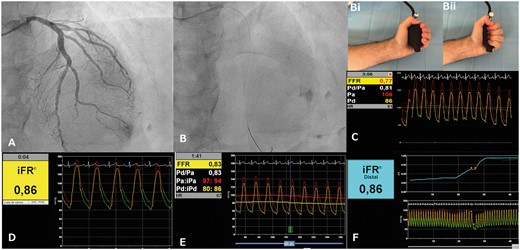
This case highlights the benefit of combining isometric exercise and coronary physiology in explaining persistent angina after percutaneous coronary intervention angina. MBs provide a unique challenge, as they are dynamic stenoses dependent on the degree of extravascular compression and intramyocardial tension. Assessment of resting physiology alone does not adequately assess the haemodynamic relevance of the MB during situations of increased inotropism. Of interest, the initial iFR of 0.86 suggested that the MB was haemodynamically significant, perhaps by limiting physiological interrogation to diastole. Compression of the epicardial segment by the MB increases intracoronary systolic pressure, and this may affect FFR values as they are obtained from whole-cycle, averaged pressure values, while iFR is obtained during diastole alone.